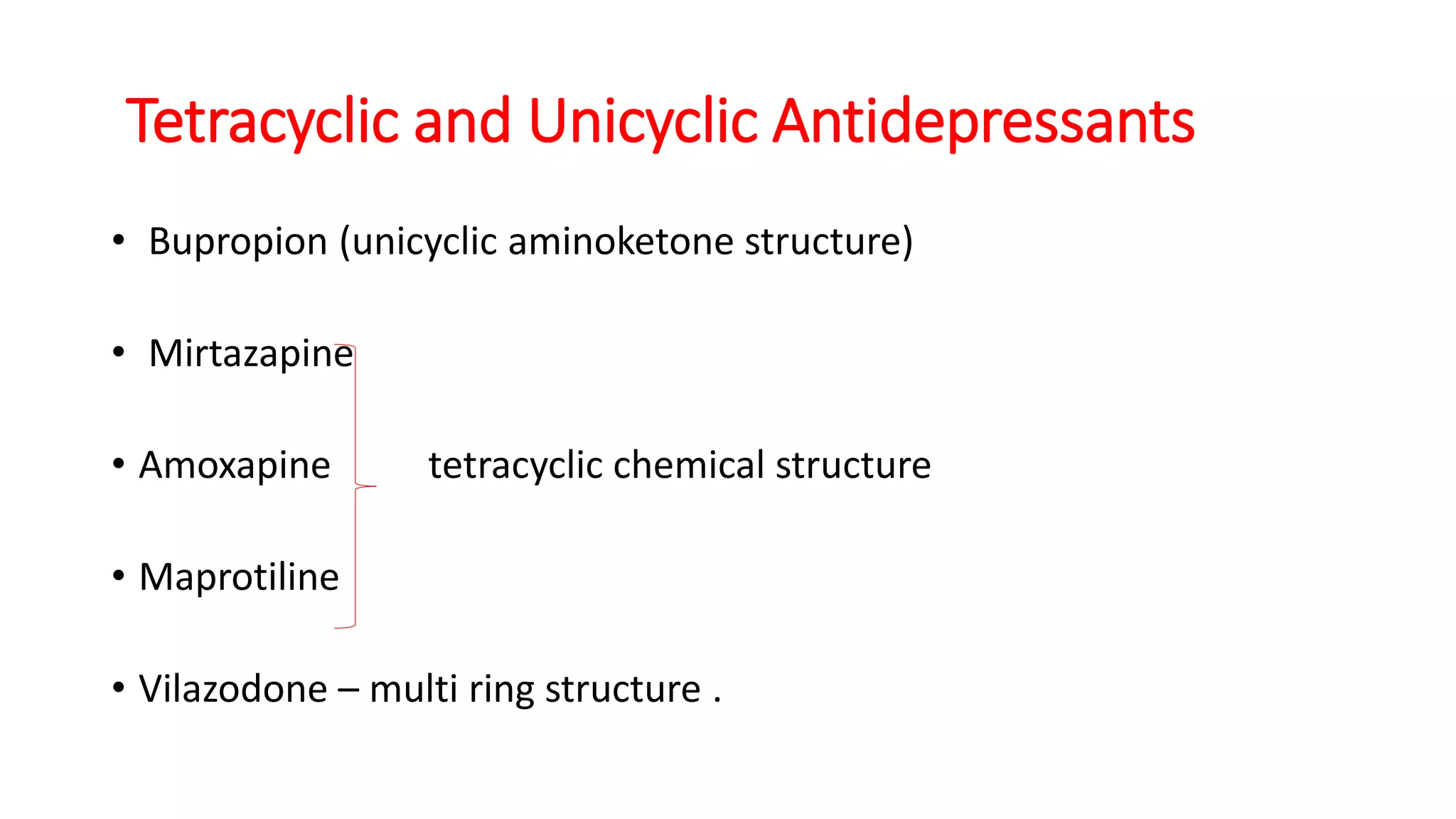
This document summarizes the pharmacotherapy of depression. It discusses the major classifications of antidepressants including SSRIs, SNRIs, TCAs, and others. It covers the pathophysiology of depression including the monoamine and neurotrophic hypotheses. For each class of antidepressant, it describes the pharmacokinetics, pharmacodynamics, dosing ranges, adverse effects, and drug interactions. CYP enzyme metabolism is an important factor in antidepressant interactions. The document provides a comprehensive overview of antidepressant treatment of depression and other conditions.