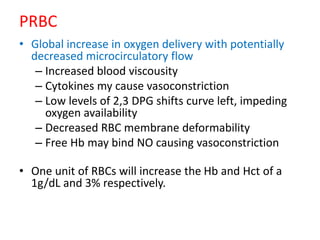
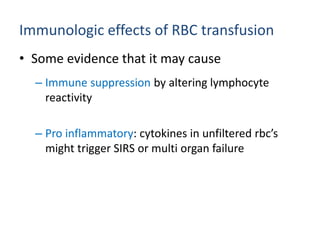
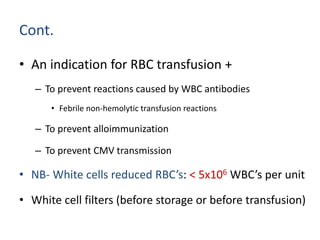
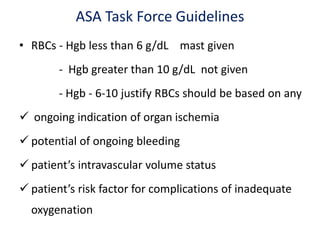
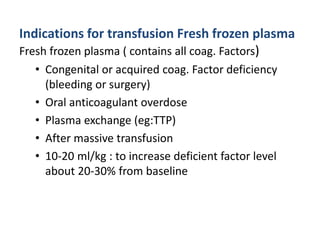
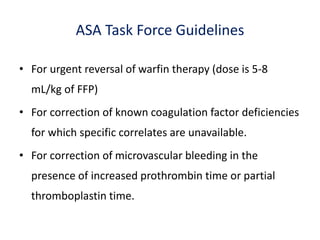
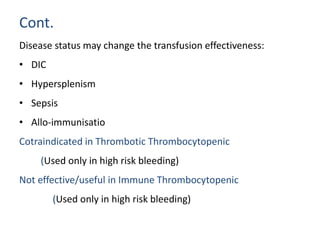
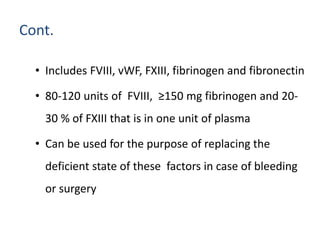
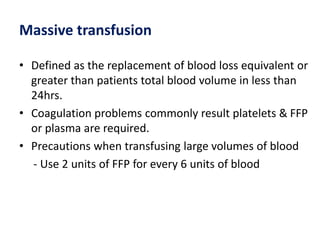
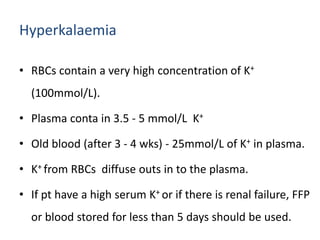
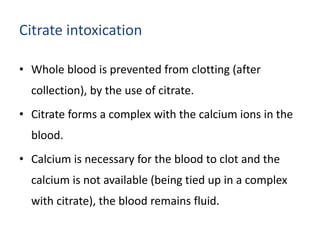
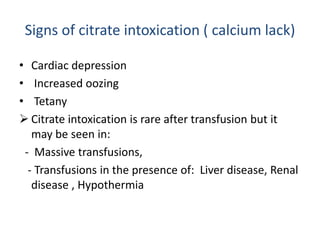
Blood transfusion involves introducing donor blood into a recipient's bloodstream. It is used to increase oxygen-carrying capacity, reverse tissue hypoxia, restore circulating volume, and provide clotting factors. Blood products include whole blood, packed red blood cells, platelets, fresh frozen plasma, and cryoprecipitate. Transfusions aim to treat anemia and coagulation disorders while minimizing complications like reactions, infections, or electrolyte abnormalities through careful screening, storage, and monitoring during the procedure.