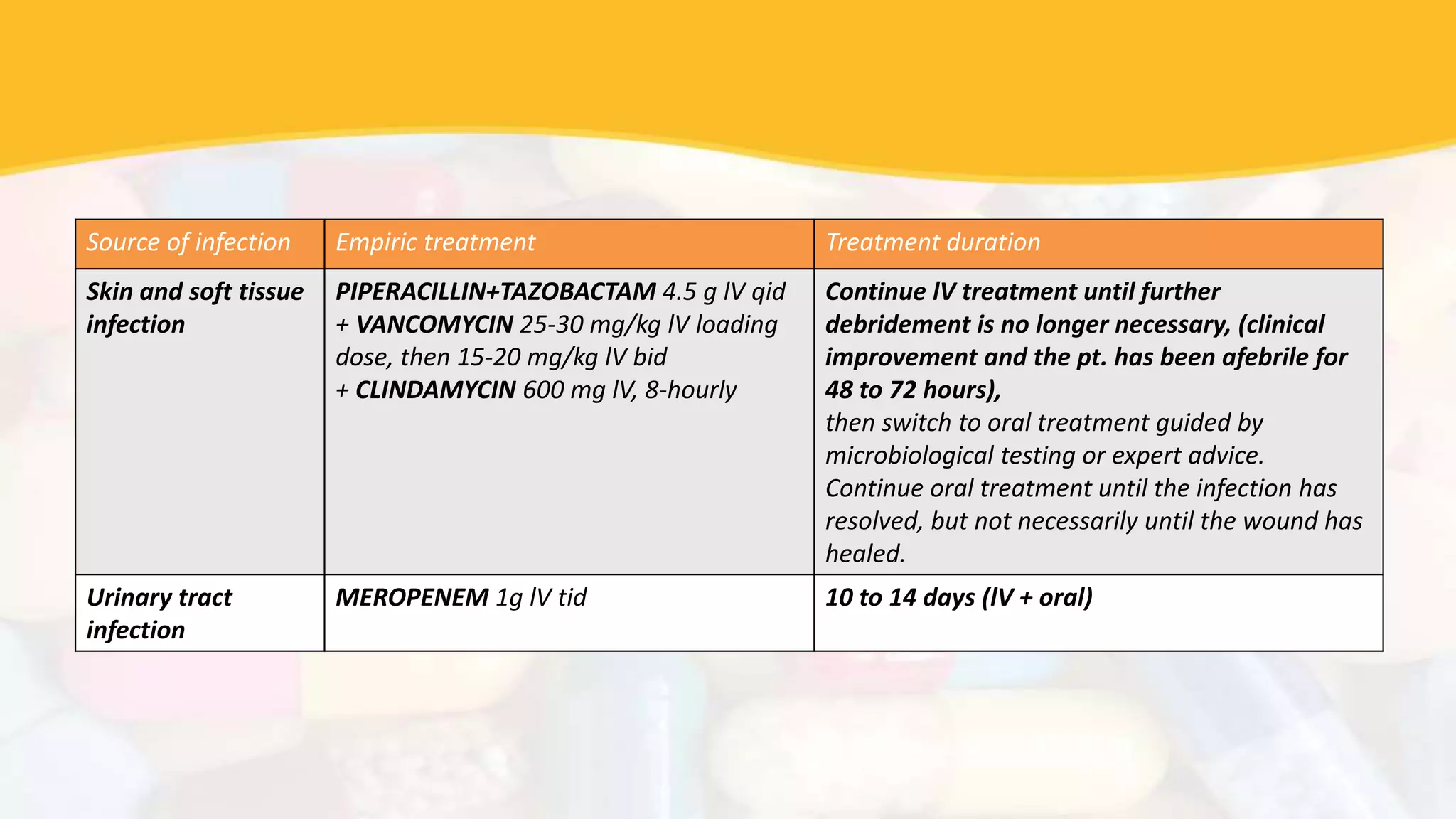
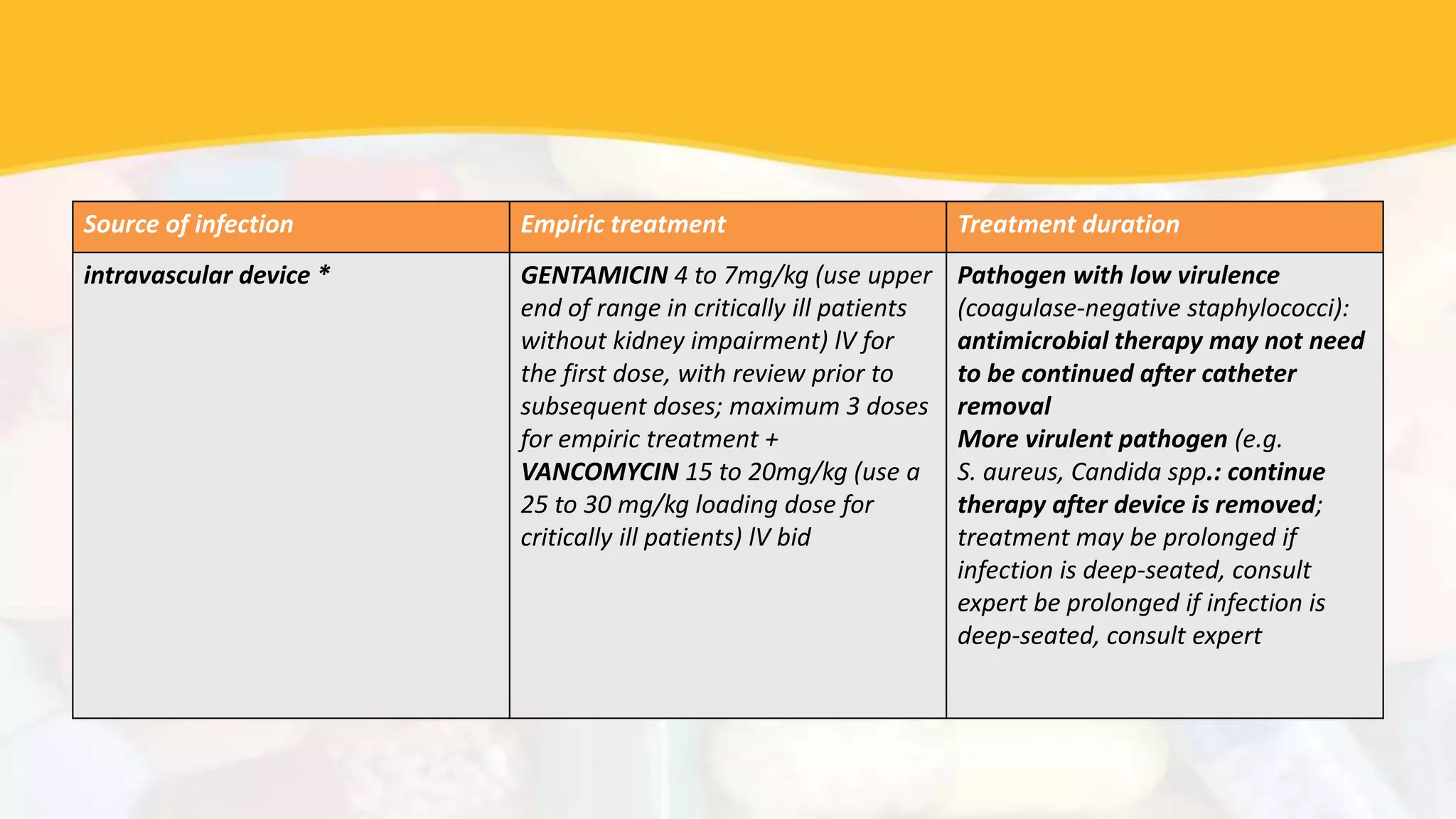
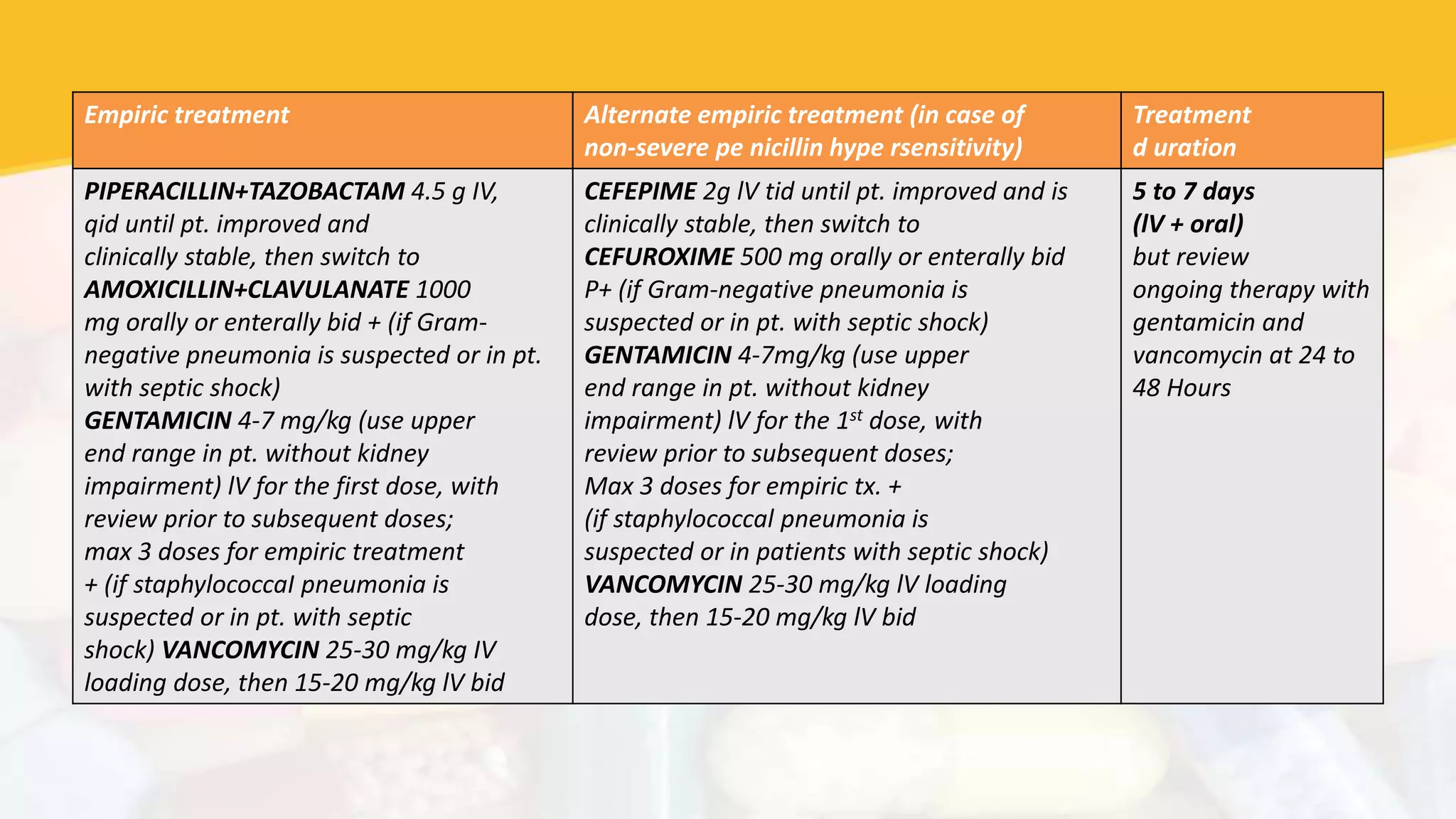
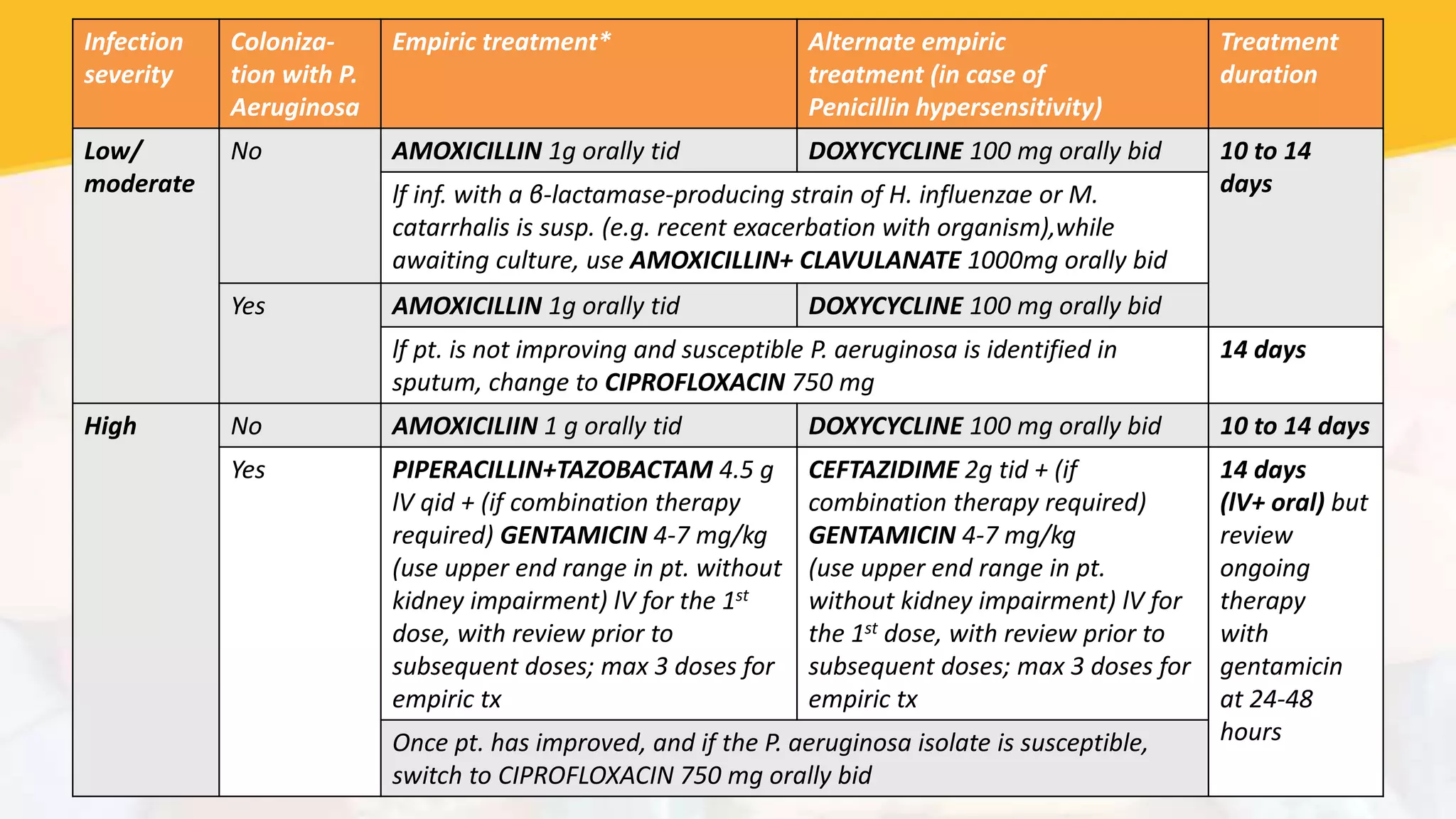
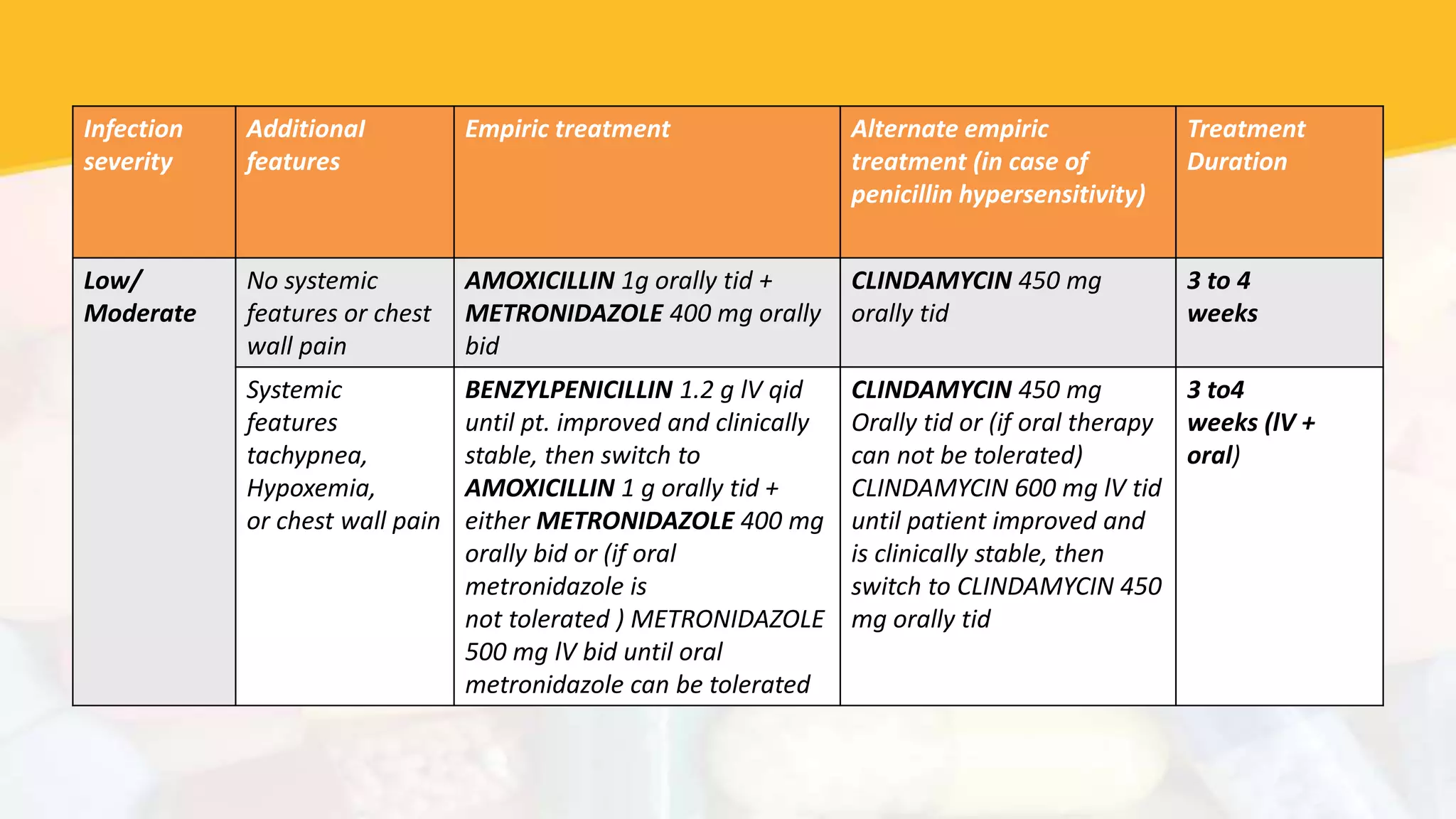
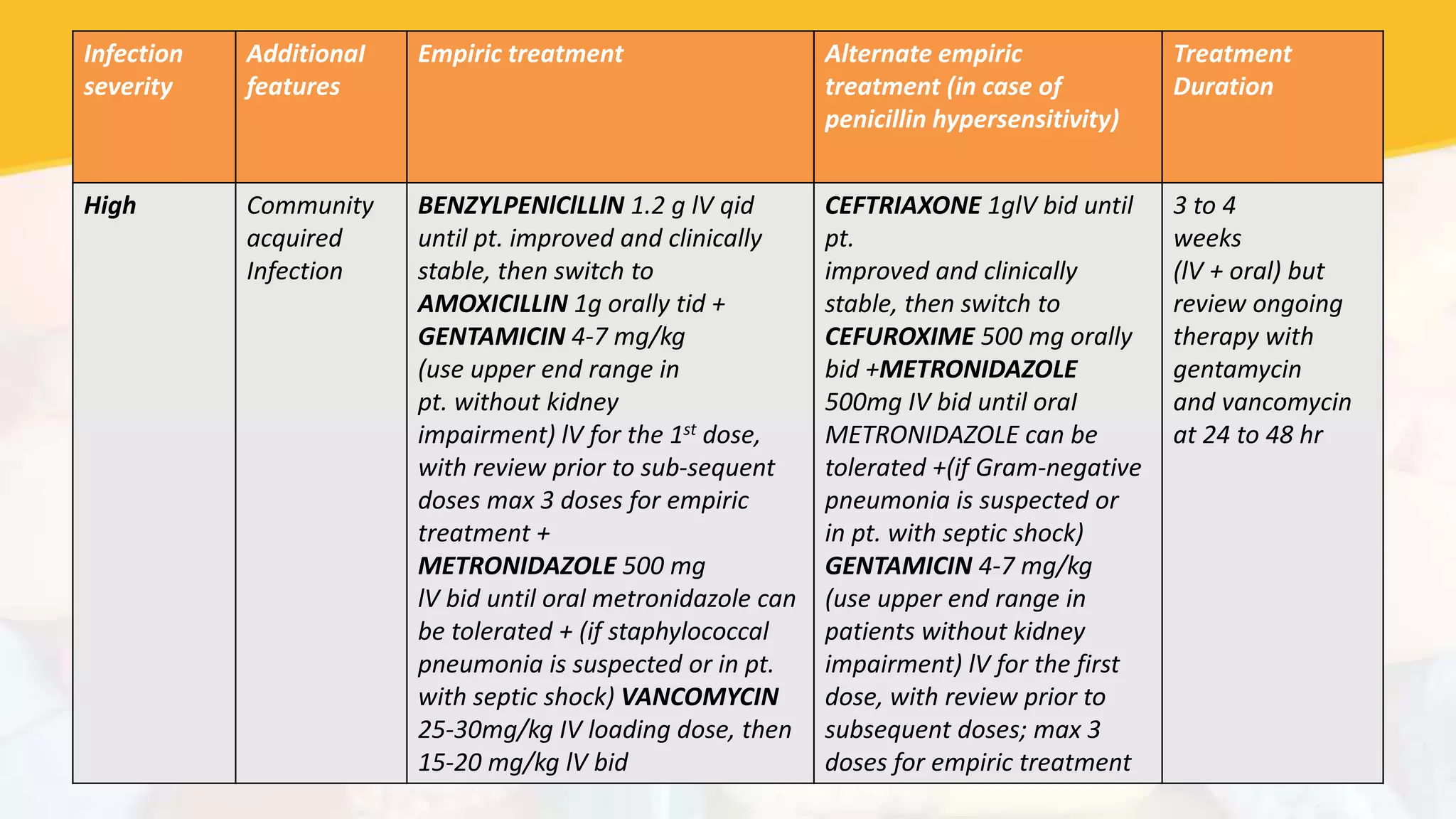
The document provides guidelines for parenteral to oral conversion of antibiotics, antibiotic treatment protocols for various infections, and considerations for antibiotic stewardship. It discusses converting IV antibiotics to oral when patients are clinically improving after 48 hours on IV regimen if they can tolerate oral medications. For treatment of infections like pneumonia and bloodstream infections, it recommends broad-spectrum IV antibiotics like meropenem or piperacillin-tazobactam along with antibiotics like vancomycin or azithromycin based on severity and suspected pathogens. It stresses the importance of de-escalating antibiotics when possible and considering the AWaRe antibiotic classification of Watch and Reserve antibiotics for more resistant infections.