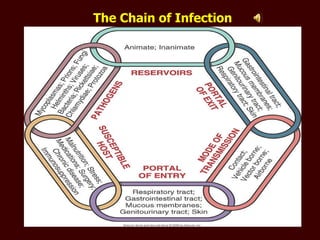
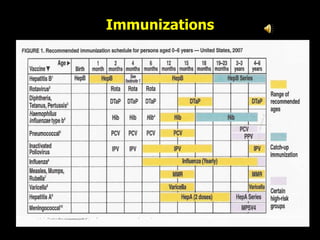
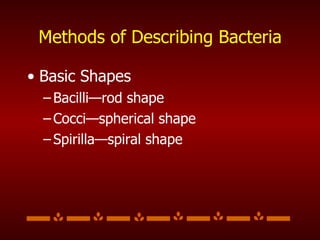
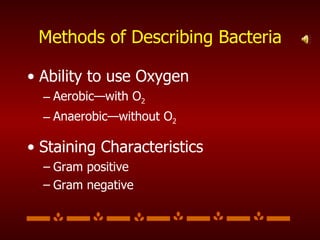
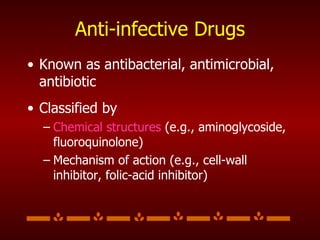
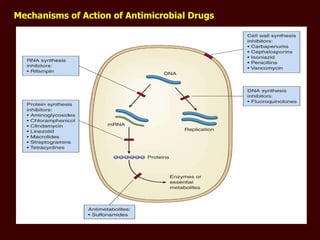
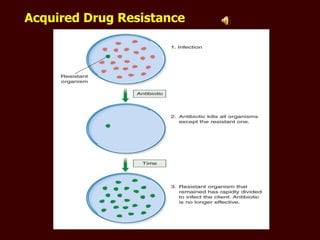
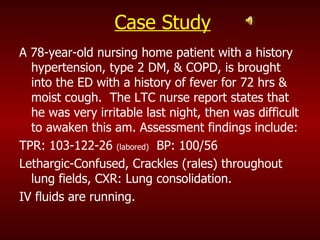
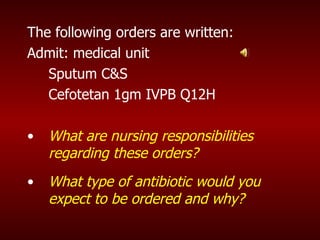
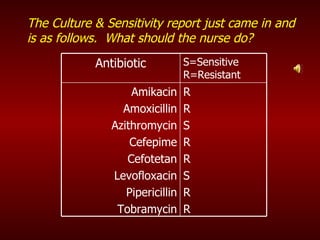
The document discusses infection and the infectious process. It defines key terms like pathogens, virulence, and susceptibility. It describes the chain of infection and factors that influence susceptibility. It also discusses infection control methods like hand hygiene, immunizations, and multidrug-resistant infections. Nursing responsibilities in managing infections include assessing patients, administering antibiotics, providing treatments and education.