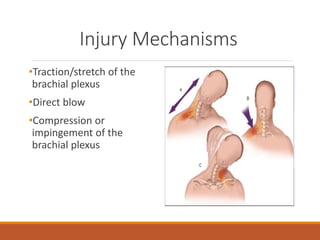
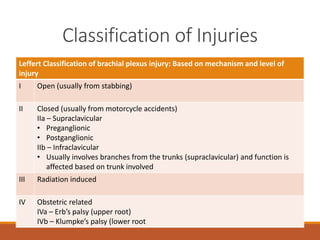
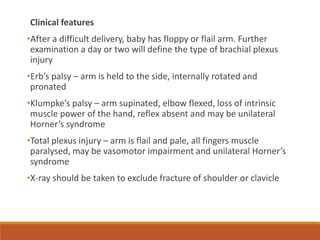
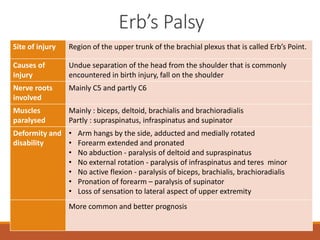
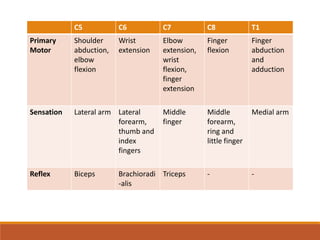
The document discusses brachial plexus injuries, which involve damage to the network of nerves that control the arm and hand. It describes the anatomy of the brachial plexus and the mechanisms, classifications, signs and symptoms, investigations, and management of both adult and obstetric brachial plexus injuries. Specific injuries like Erb's palsy and Klumpke's palsy are also explained. The prognosis depends on the level and severity of the injury, with upper plexus injuries having a better prognosis than lower plexus or total plexus lesions. Early surgical intervention may be needed for severe injuries or root avulsions.