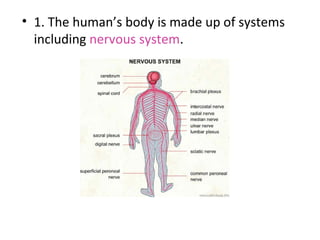
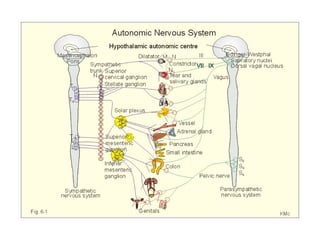
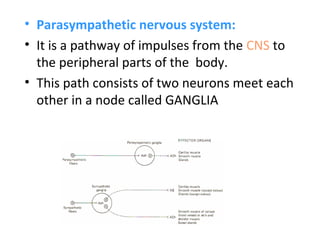
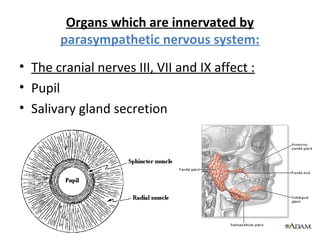
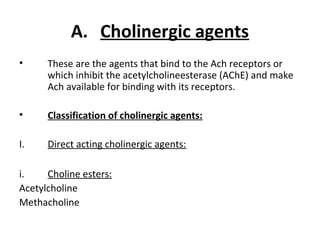
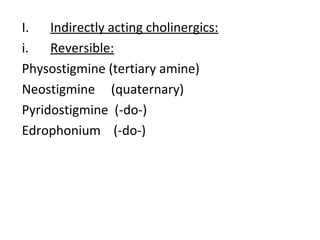
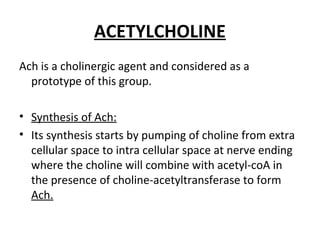
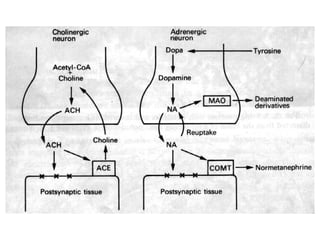
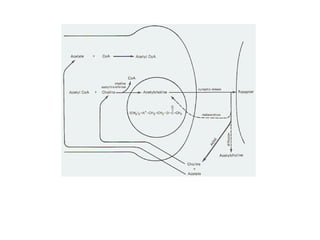
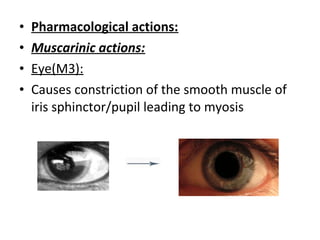
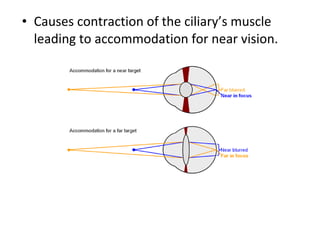
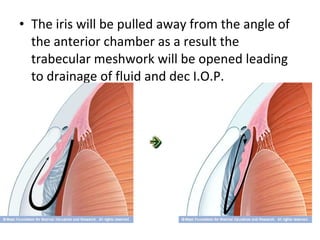
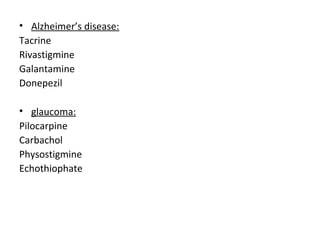
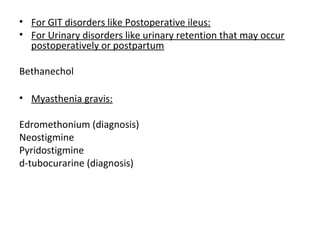
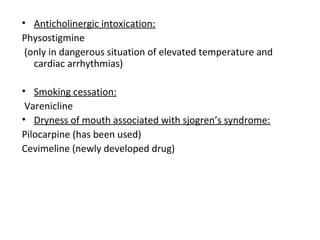
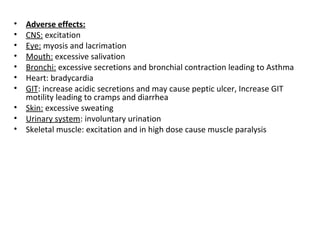
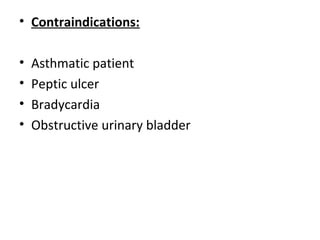
The document discusses the autonomic nervous system and autonomic drugs. It describes the parasympathetic nervous system in detail. The parasympathetic nervous system uses acetylcholine as its neurotransmitter and has effects such as reducing heart rate and blood pressure and facilitating digestion. Drugs that act on the parasympathetic nervous system are cholinergic agents, which mimic acetylcholine, and anticholinergic agents, which block acetylcholine's effects. Cholinergic drugs include acetylcholine and are used to treat conditions like Alzheimer's disease and glaucoma. Anticholinergic drugs have opposite effects and are used to treat cholinergic intoxication.