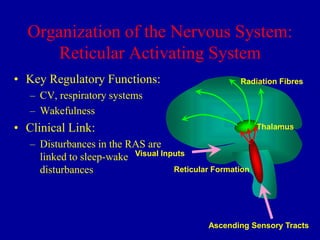
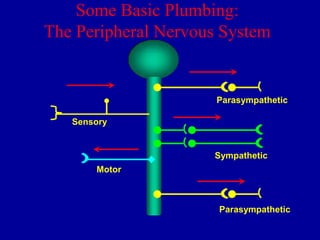
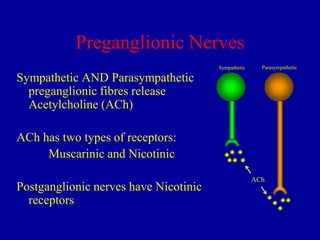
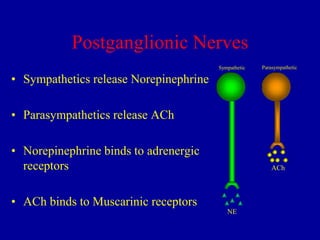
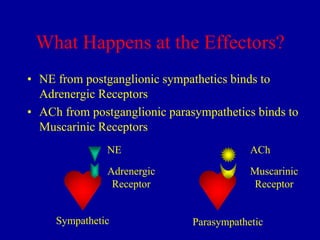
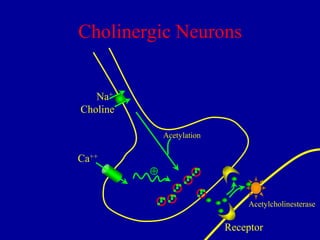
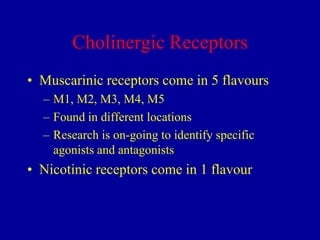
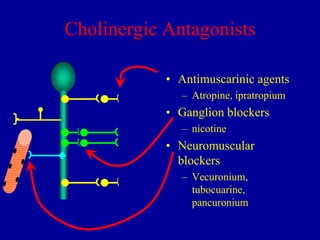
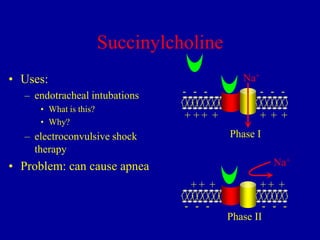
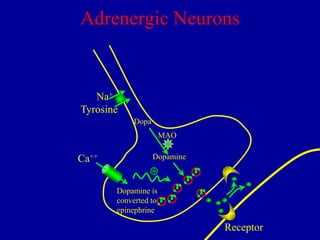
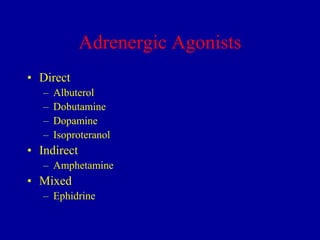
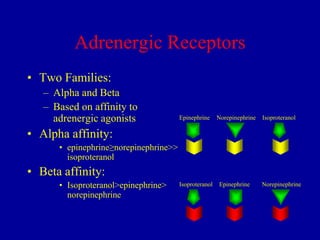
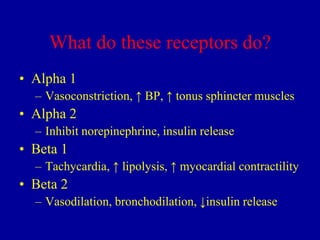
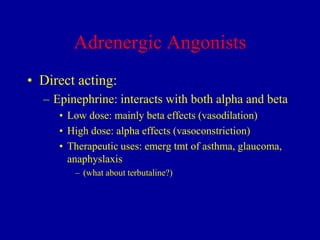
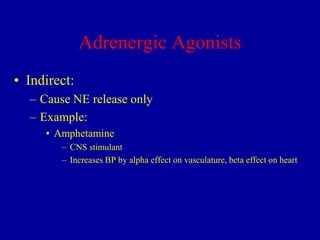
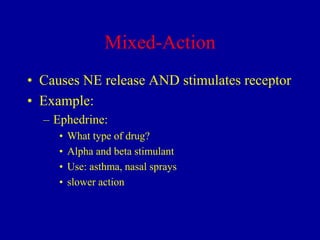
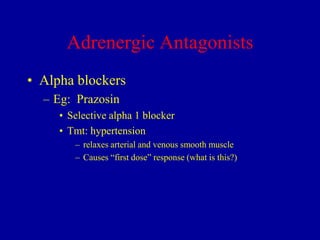
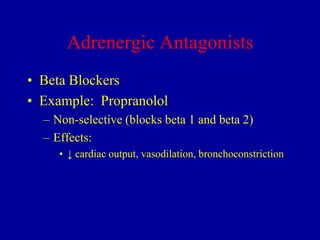
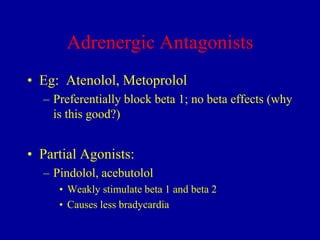
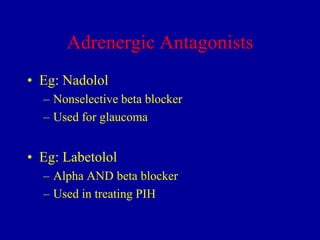
This document provides an overview of the autonomic nervous system and drugs that affect it. It begins with the organization of the central and peripheral nervous systems. It then describes the cholinergic and adrenergic systems in detail, including the receptors, neurotransmitters, and examples of agonists and antagonists. Common uses of these drugs are also outlined. The document concludes with a section on Parkinson's disease and its treatment, focusing on levodopa and other pharmacological and surgical approaches.