This document discusses various conditions affecting the ankle, including:
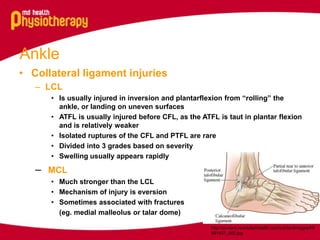
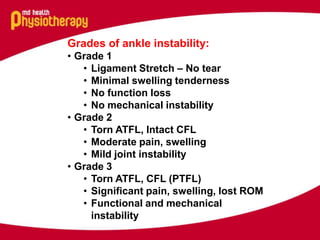
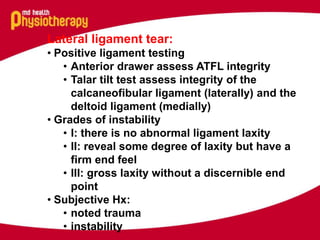
- Lateral collateral ligament injuries which can occur from ankle rolls and involve tears of the anterior talofibular ligament.
- Medial collateral ligament injuries which are stronger but can occur from eversion injuries and sometimes associated fractures.
- Anterior shin splints which result from inflammation due to overuse and repetitive impact loading.
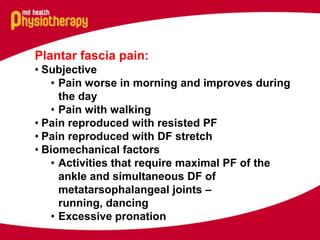
- Tibialis posterior tendinopathy which can occur from overuse and involves excessive pronation placing increased load on the tendon.
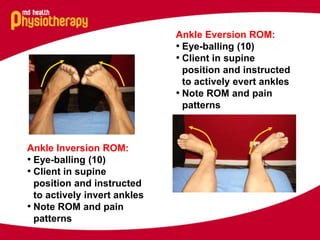
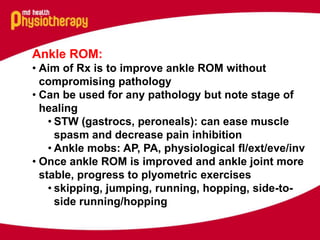
- Various assessments are described to evaluate range of motion, strength, and ligament integrity of the ankle. Treatment focuses on improving range of motion and strengthening without aggravating the