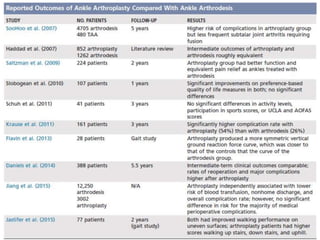
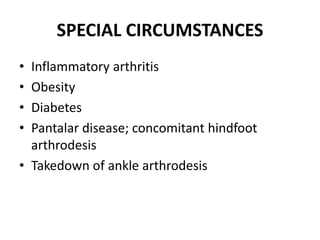
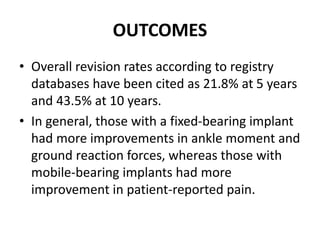
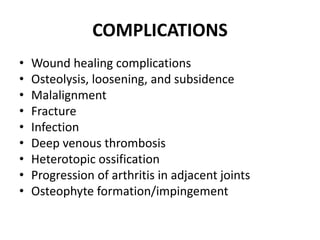
This document discusses the history and design of ankle replacement implants. It describes the evolution from first-generation constrained implants requiring extensive bone resection to current third-generation semi-constrained implants with three components. Fixed-bearing and mobile-bearing designs are compared, along with factors in determining candidacy, surgical technique, outcomes, and complications of total ankle replacement.