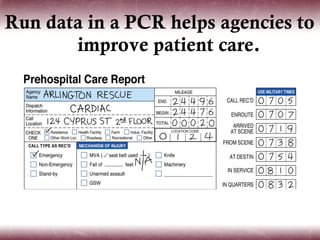
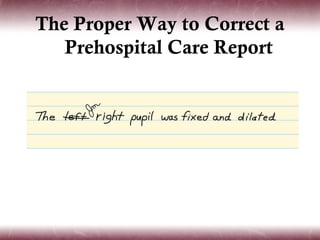
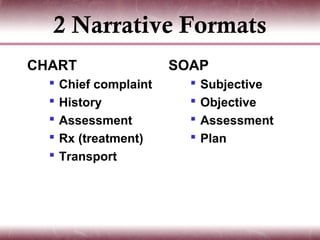
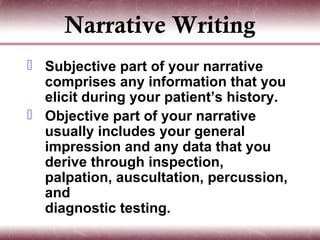
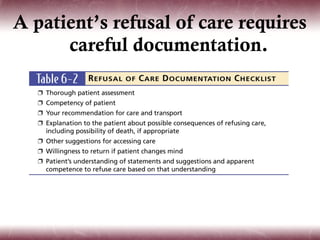
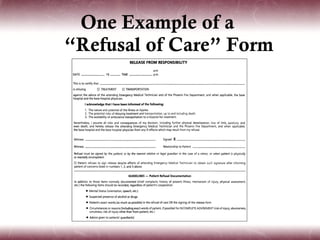
This document discusses the principles and purposes of EMS documentation. It emphasizes that the prehospital care report (PCR) is the sole written record of an ambulance call and should include both narrative and check-box sections. The PCR is used for medical, administrative, research, and legal purposes. Special situations like patient refusals, non-transport calls, and mass casualty incidents require specific documentation approaches. Proper documentation is important for patient care, legal protection, and system improvement.