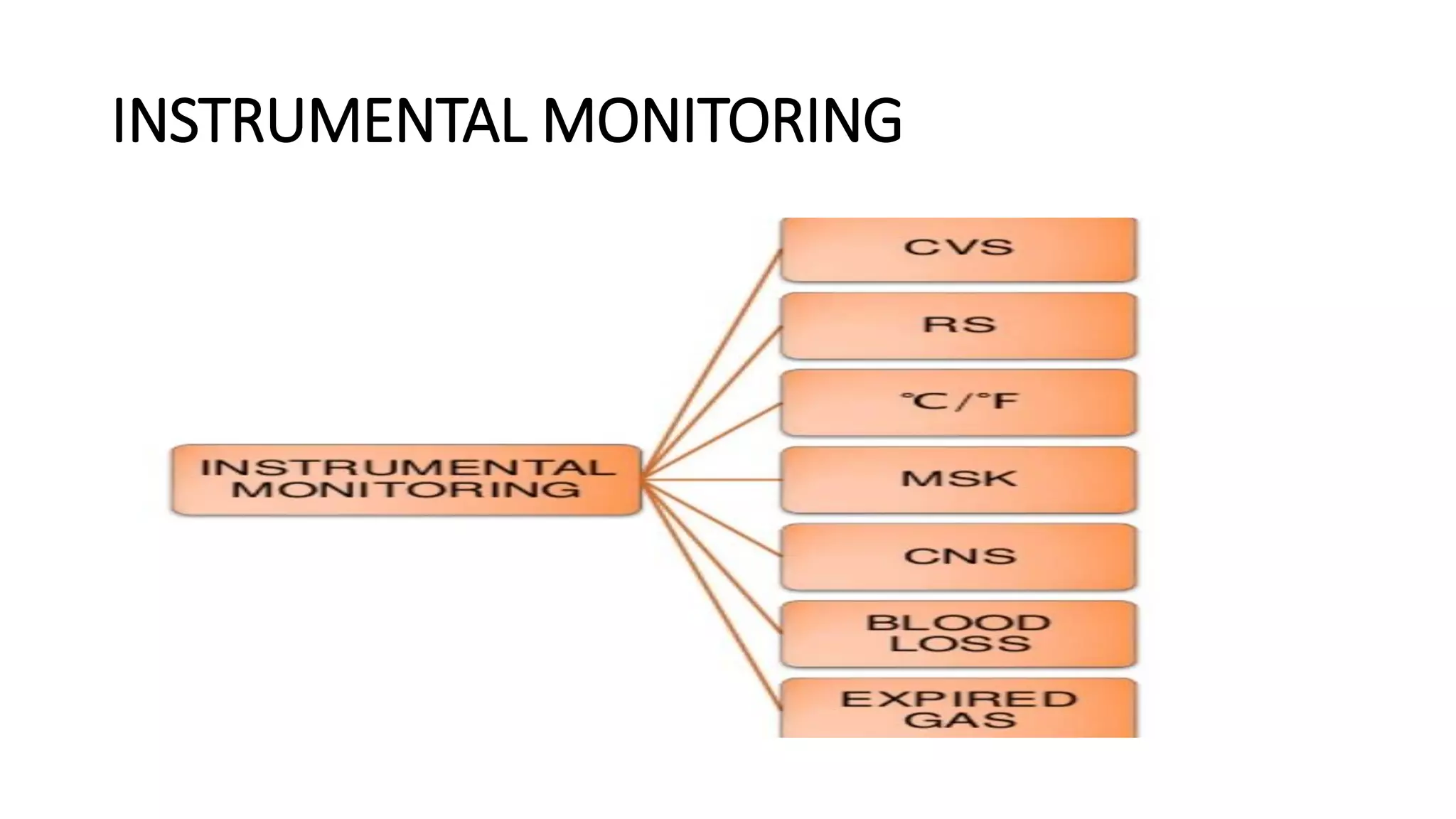
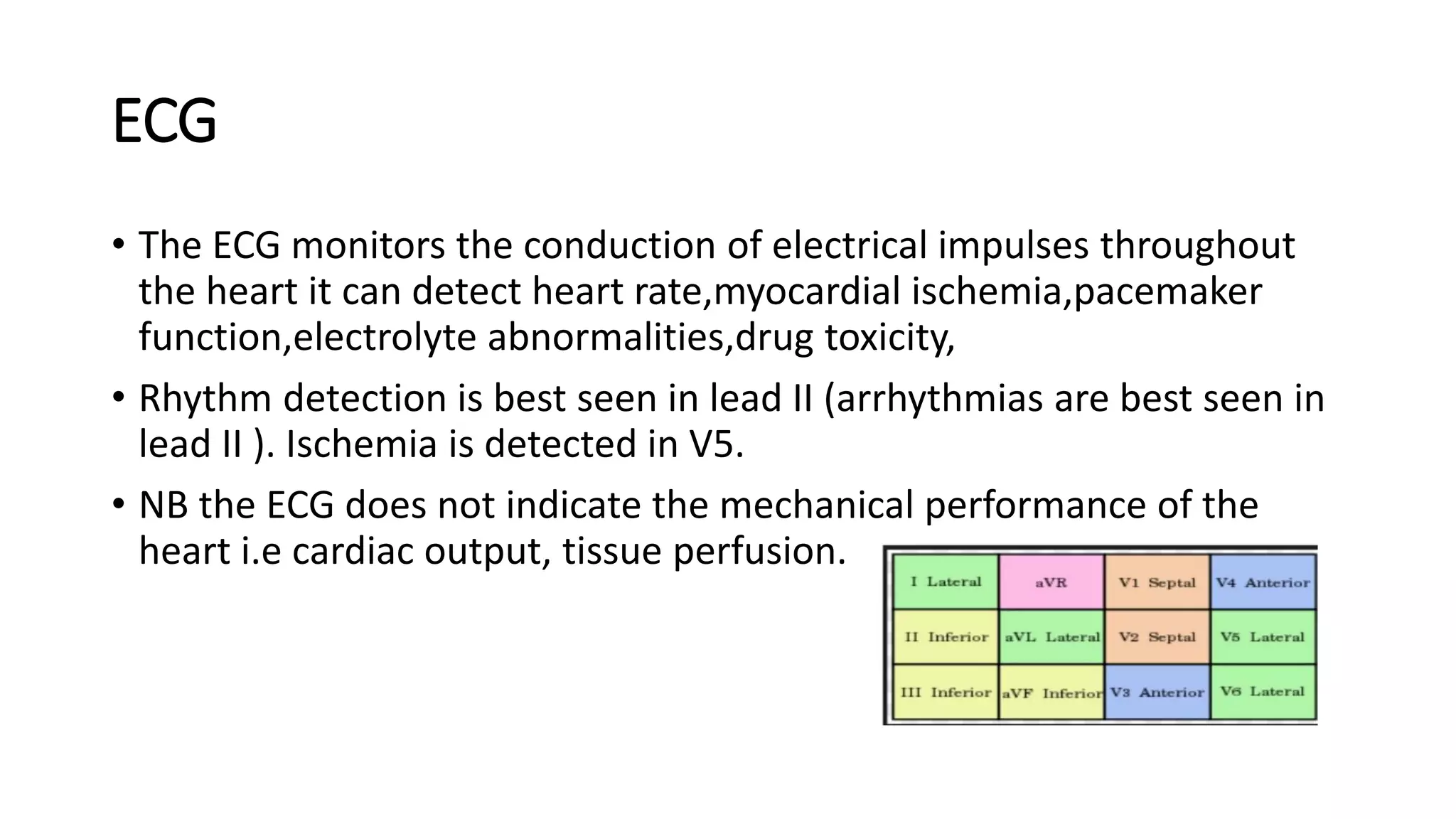
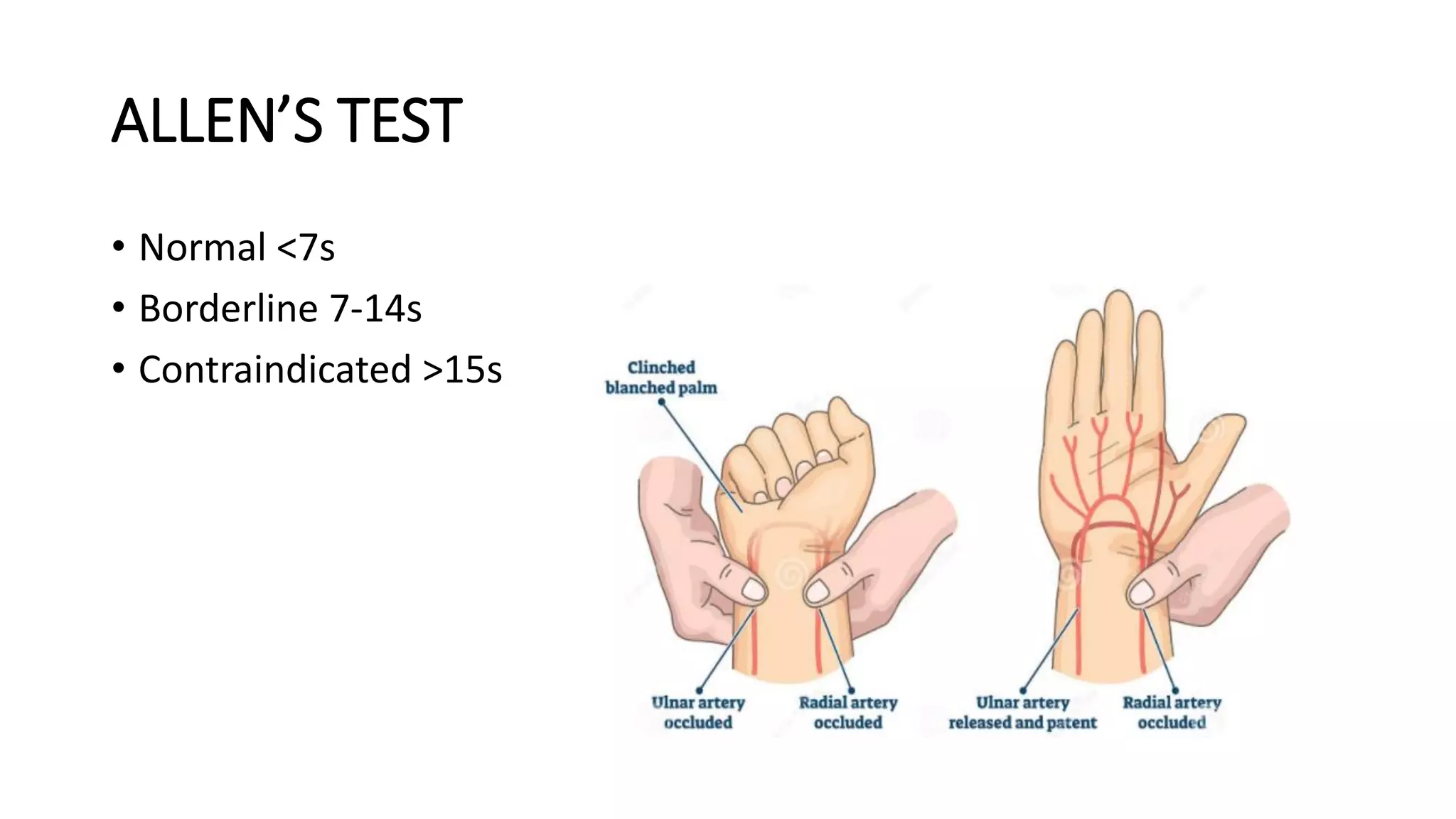
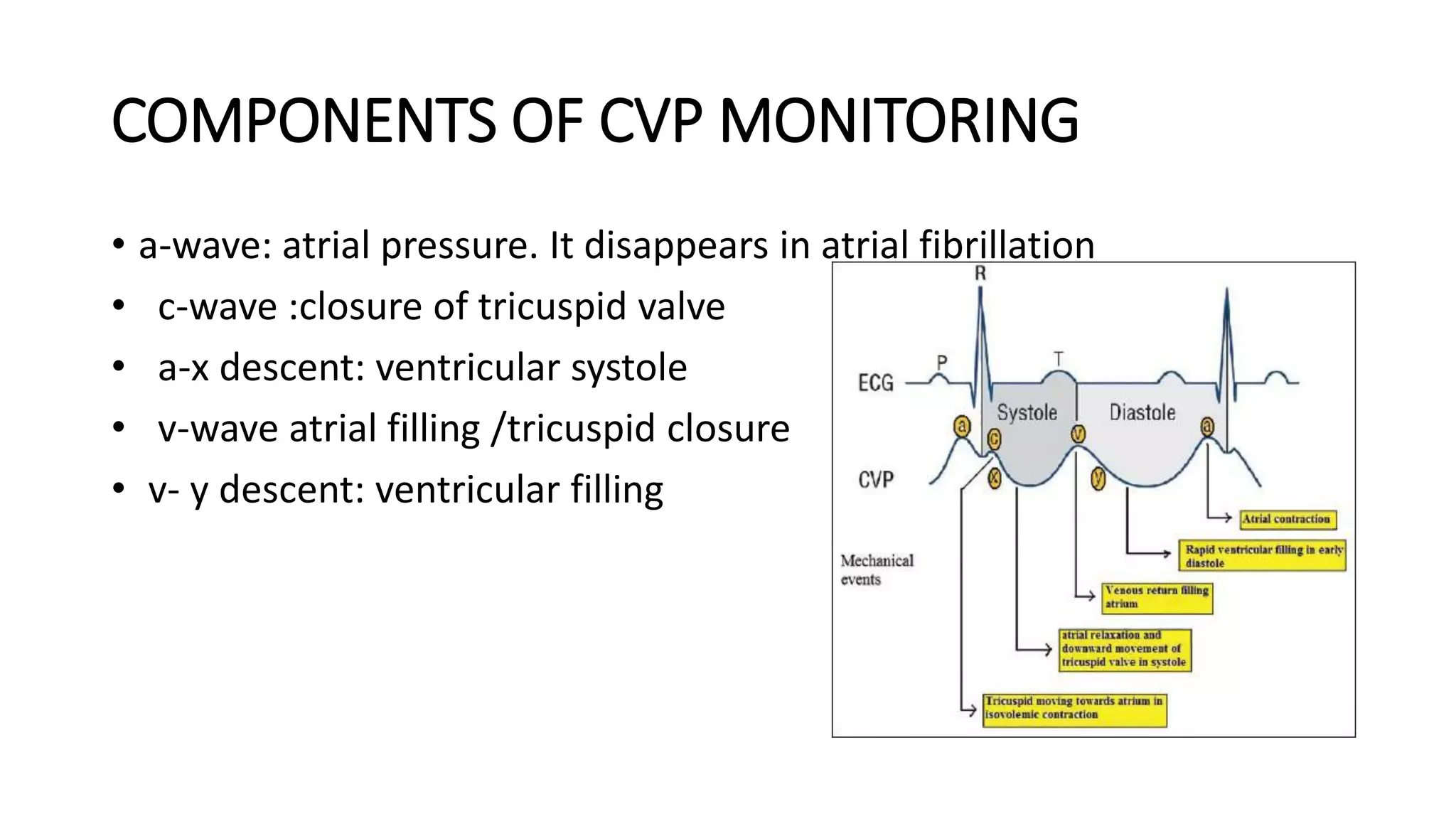
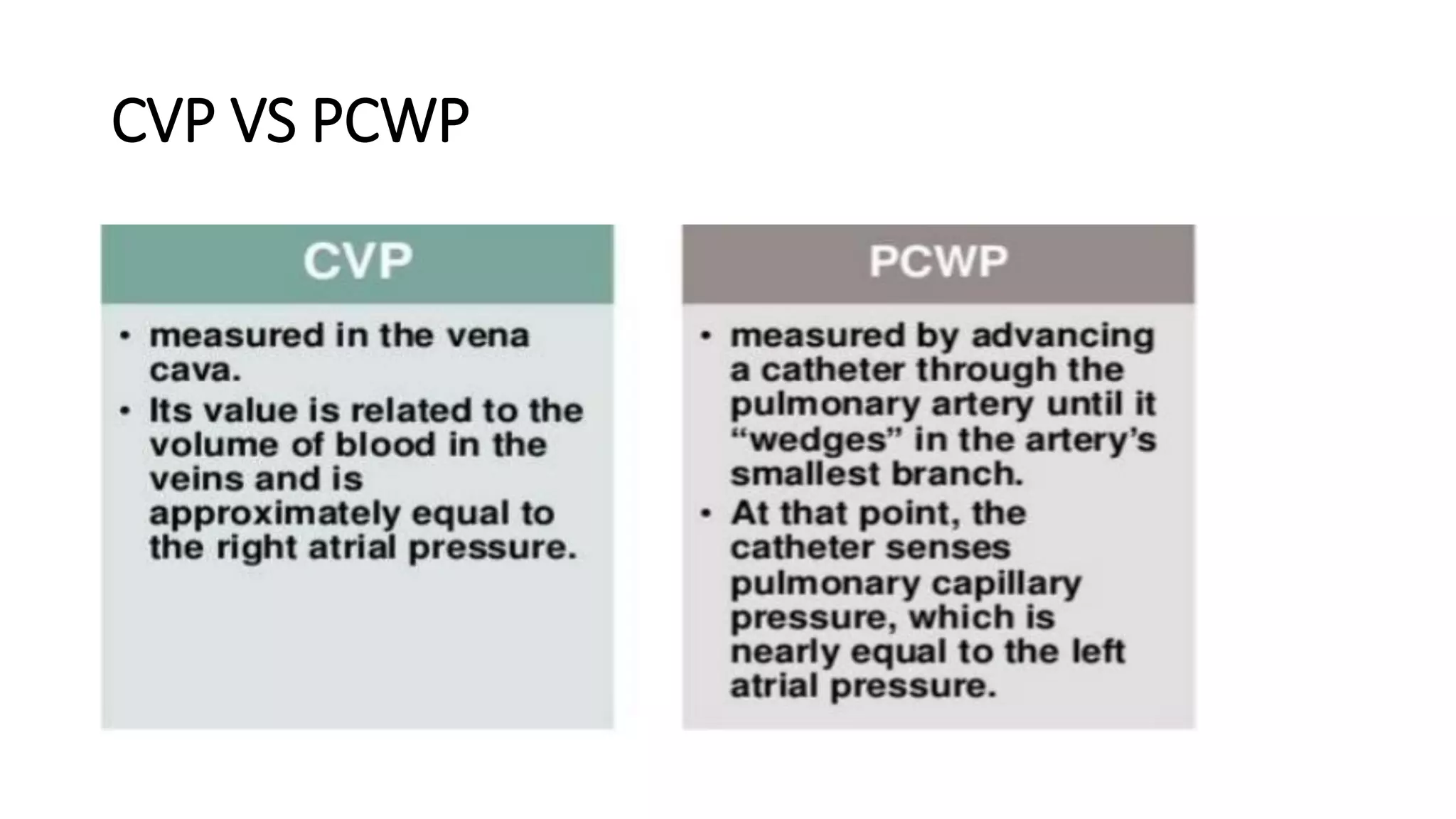
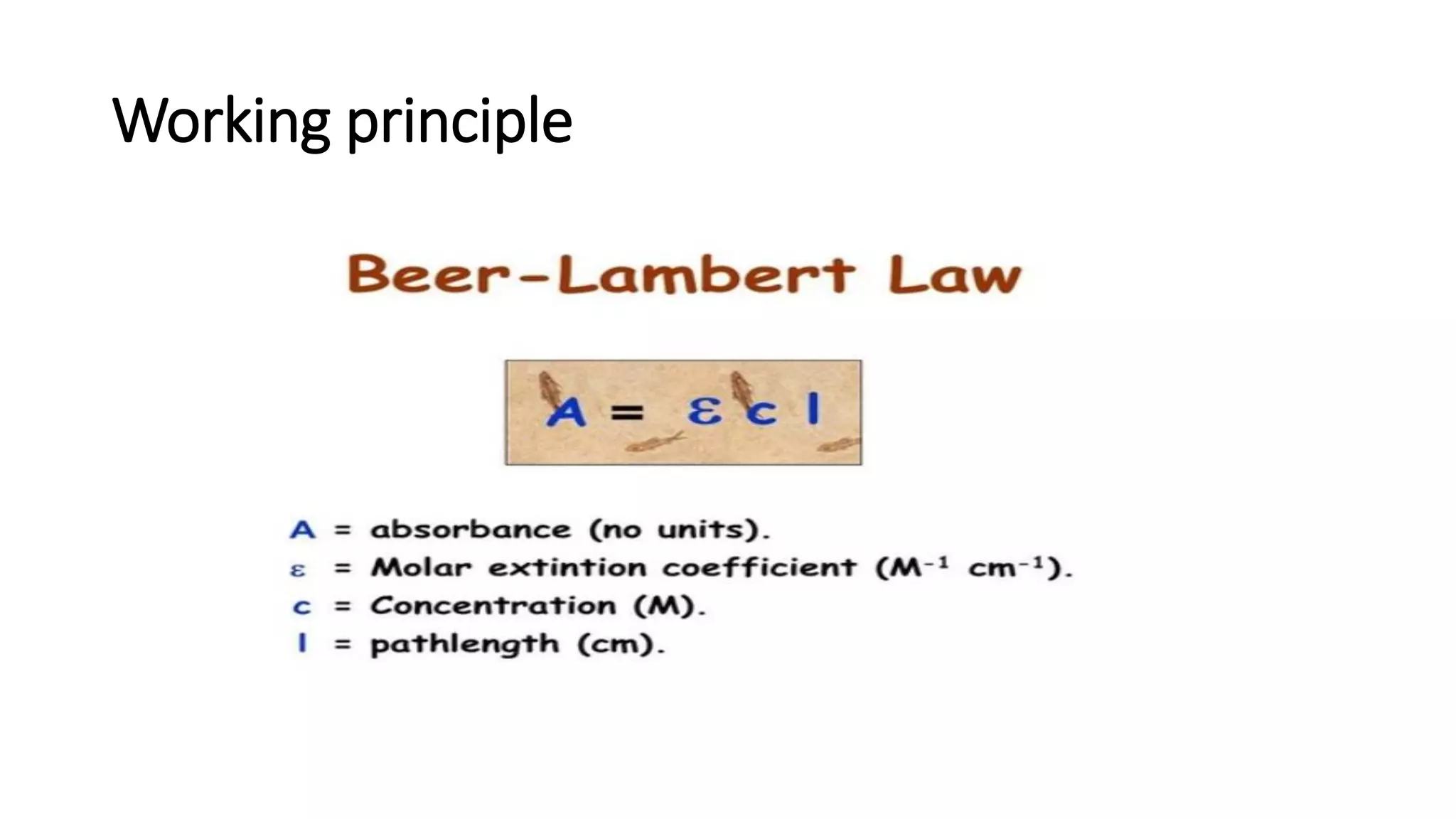
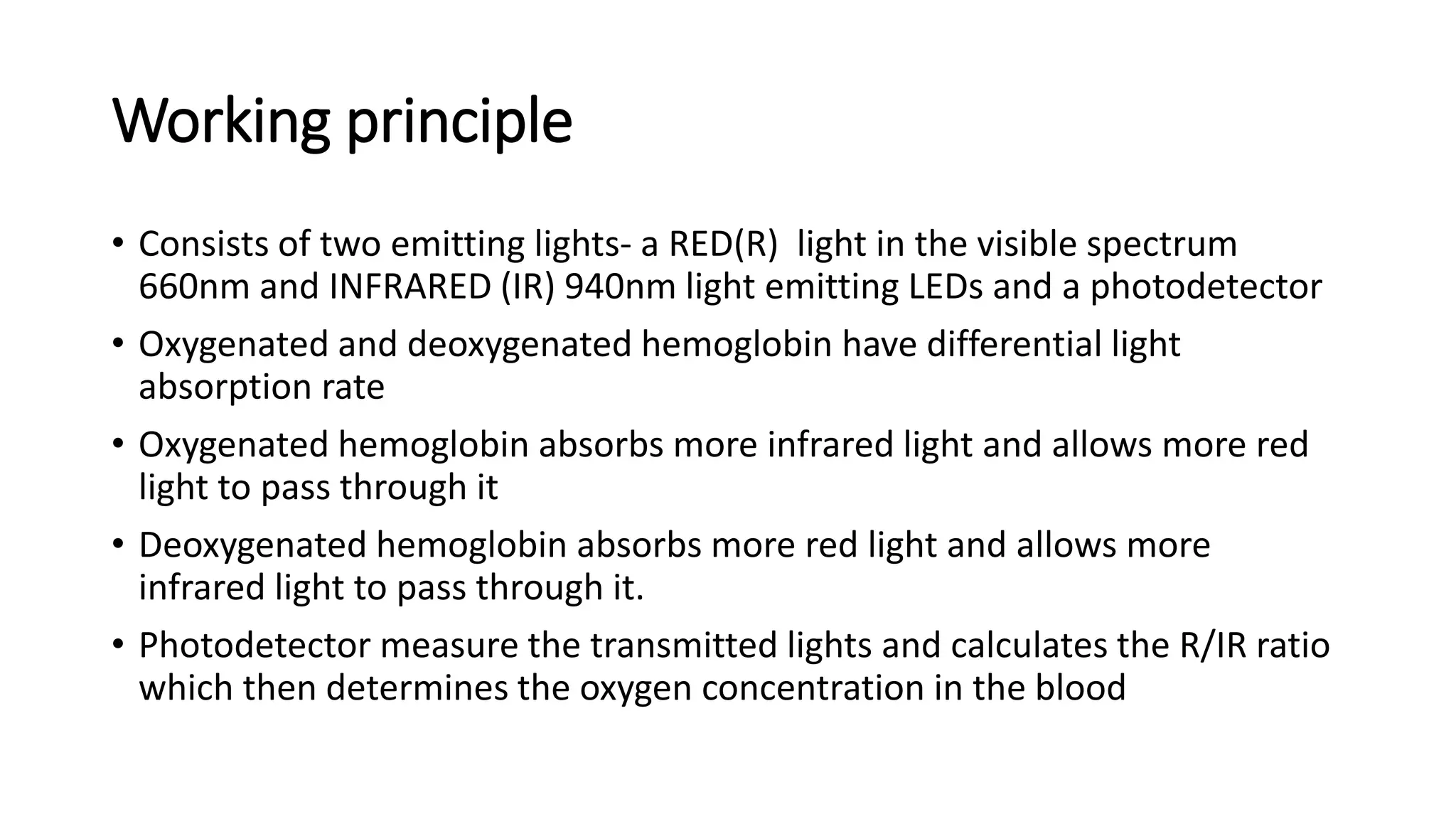
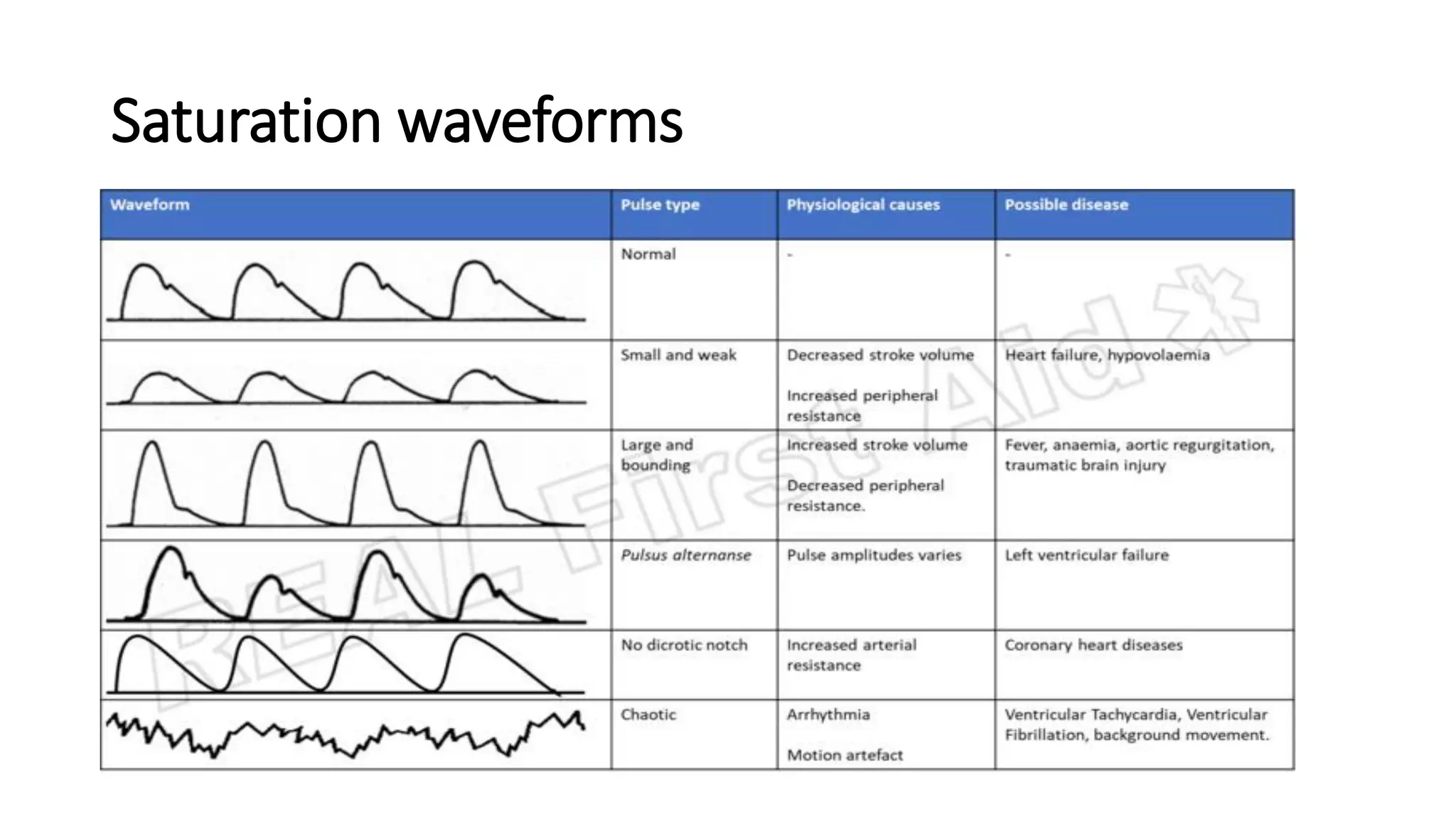
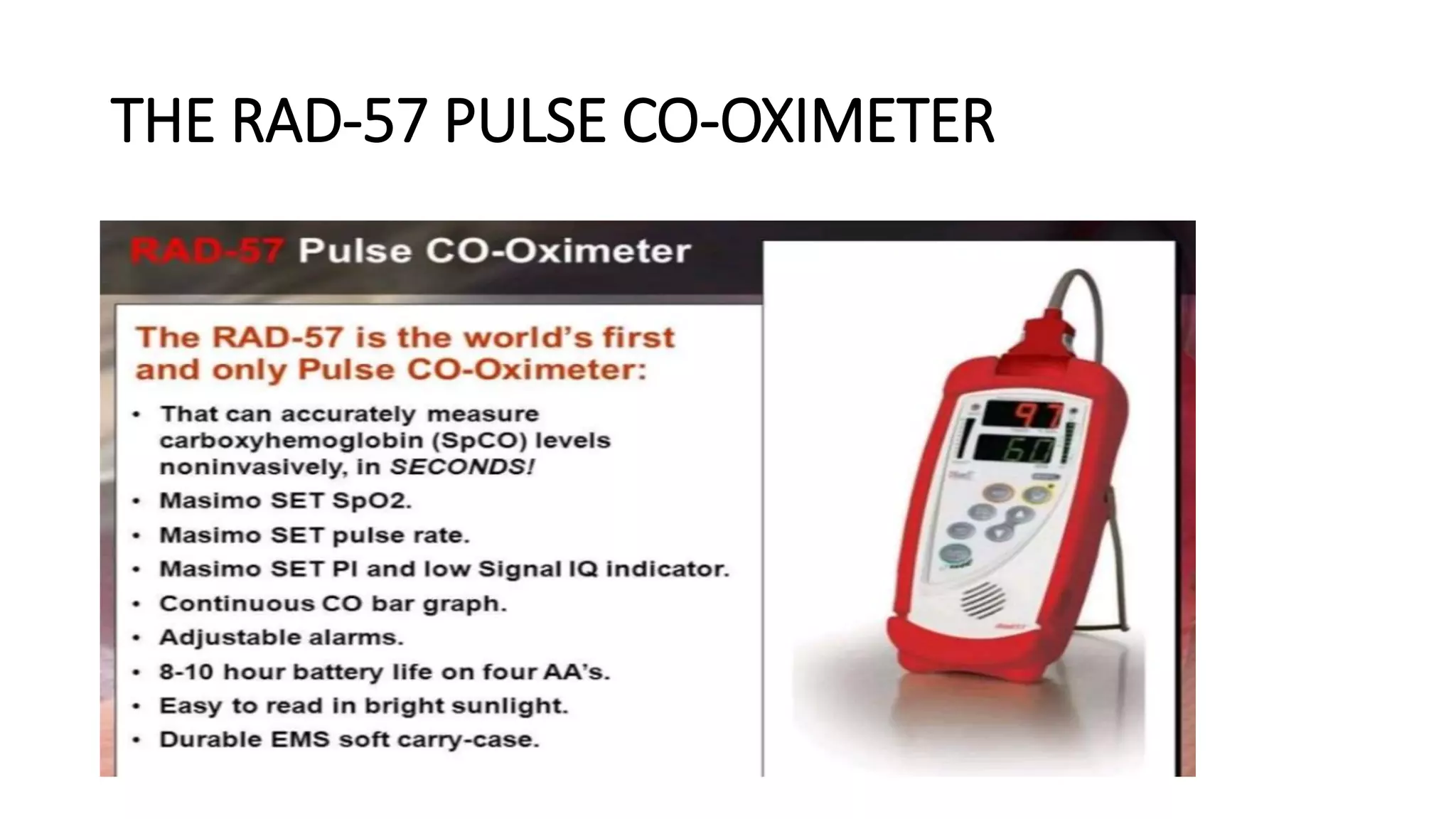
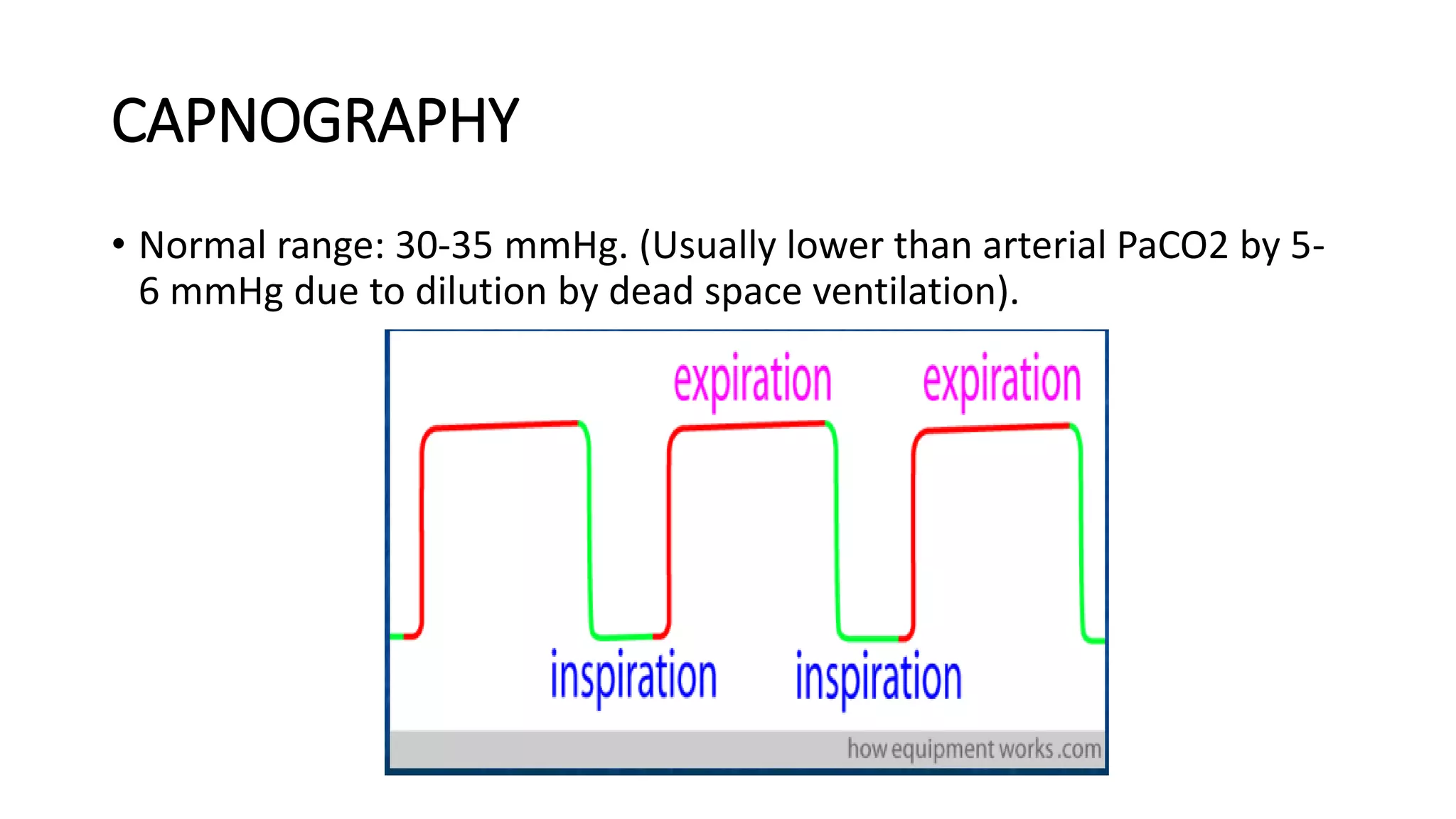
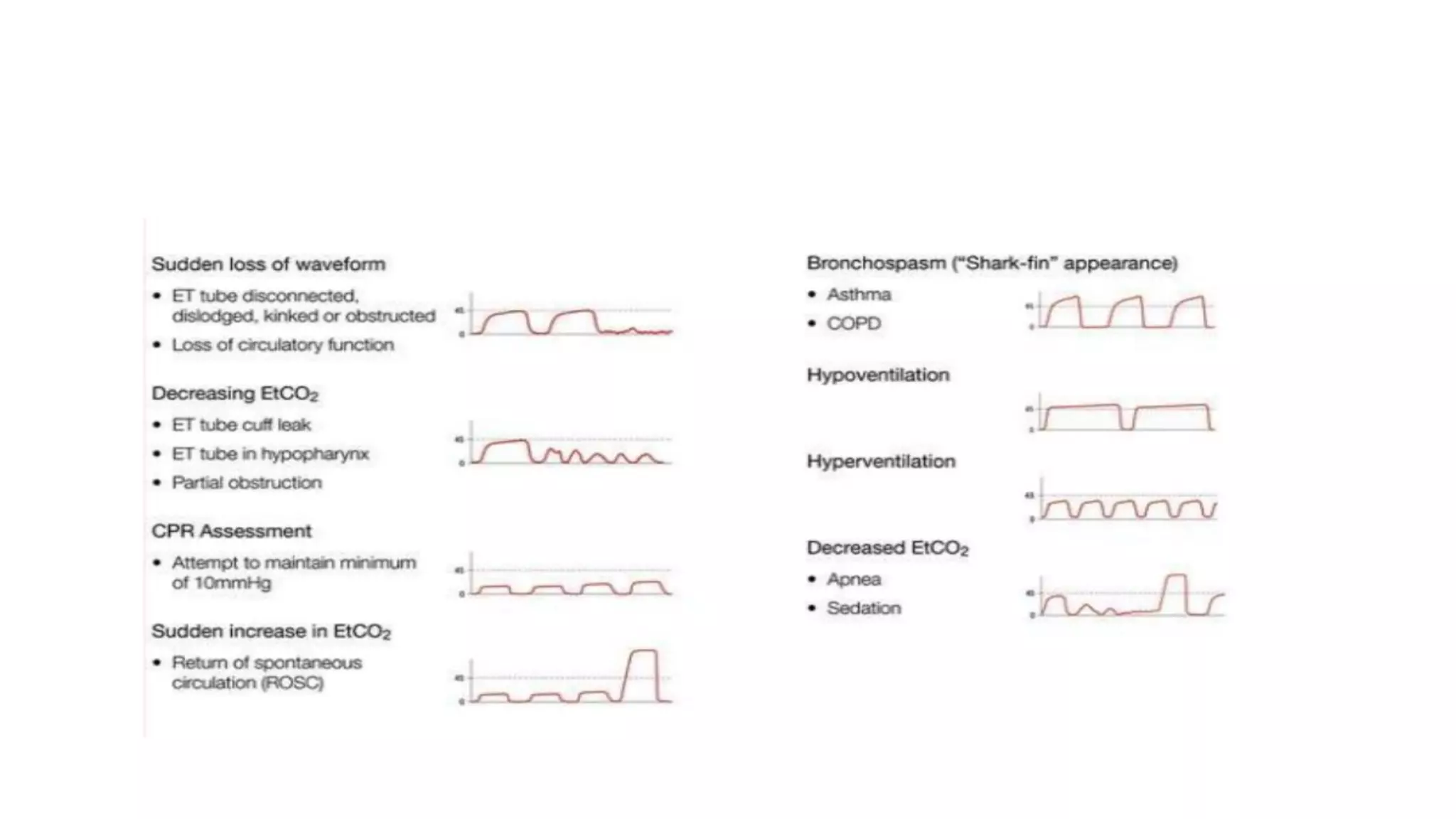
This document provides an overview of intraoperative patient monitoring. It defines monitoring as warning or recognizing issues. Key aspects of monitoring discussed include the cardiovascular, respiratory and central venous pressure systems. Specific monitoring modalities covered are ECG, blood pressure, pulse oximetry, capnography and blood gas analysis. The roles of monitoring in assessing oxygenation, ventilation and perfusion are emphasized.