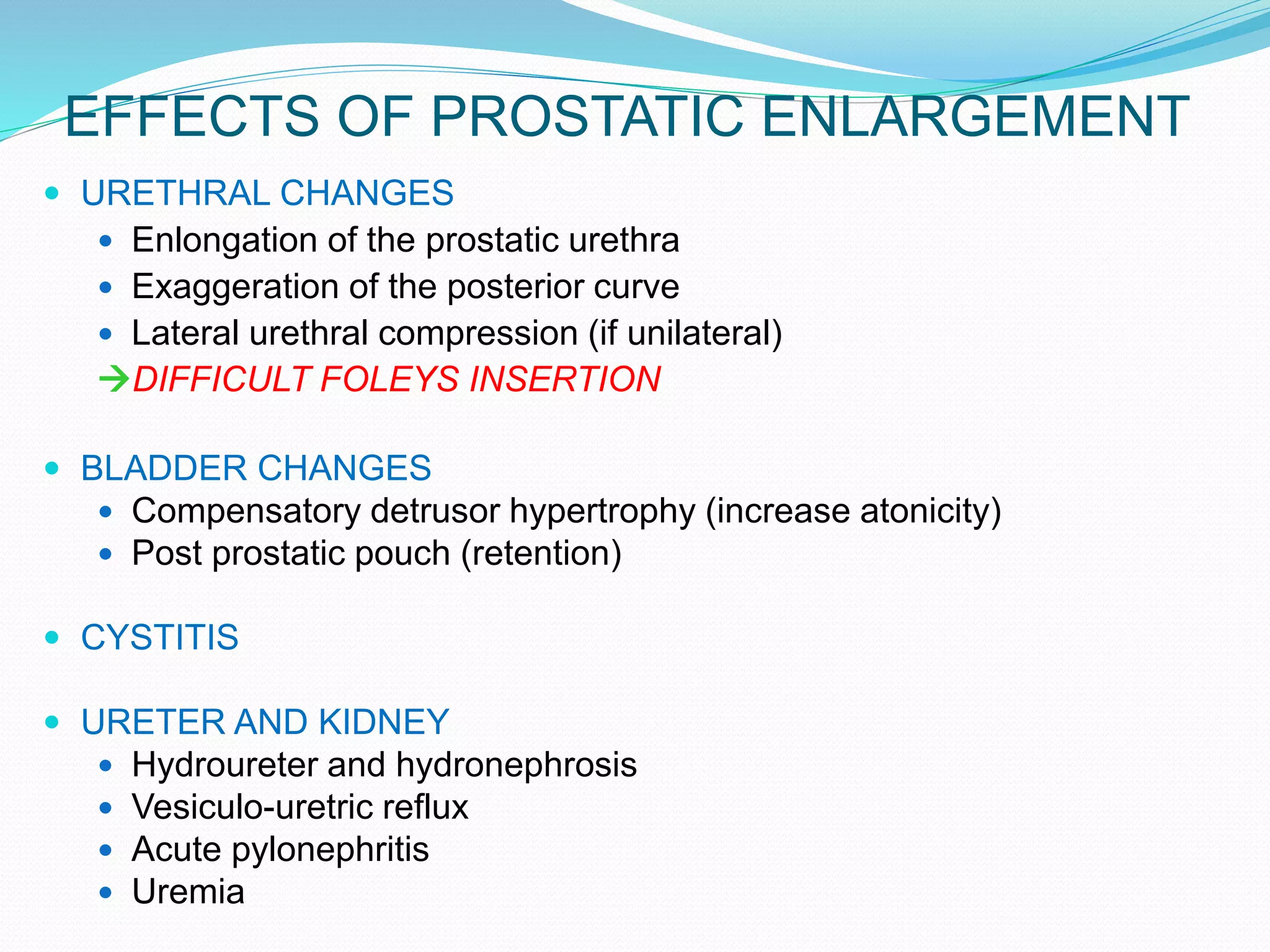
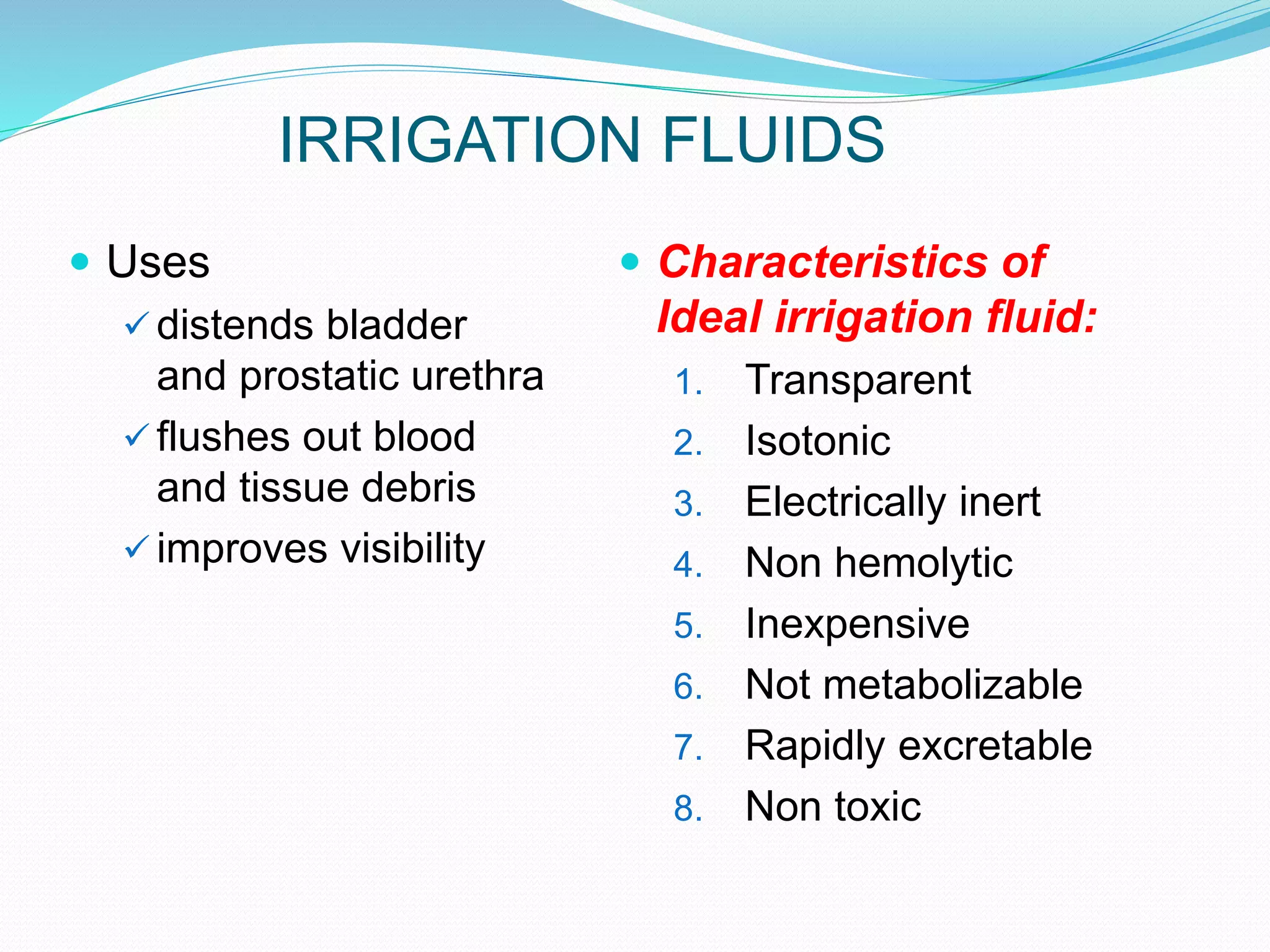
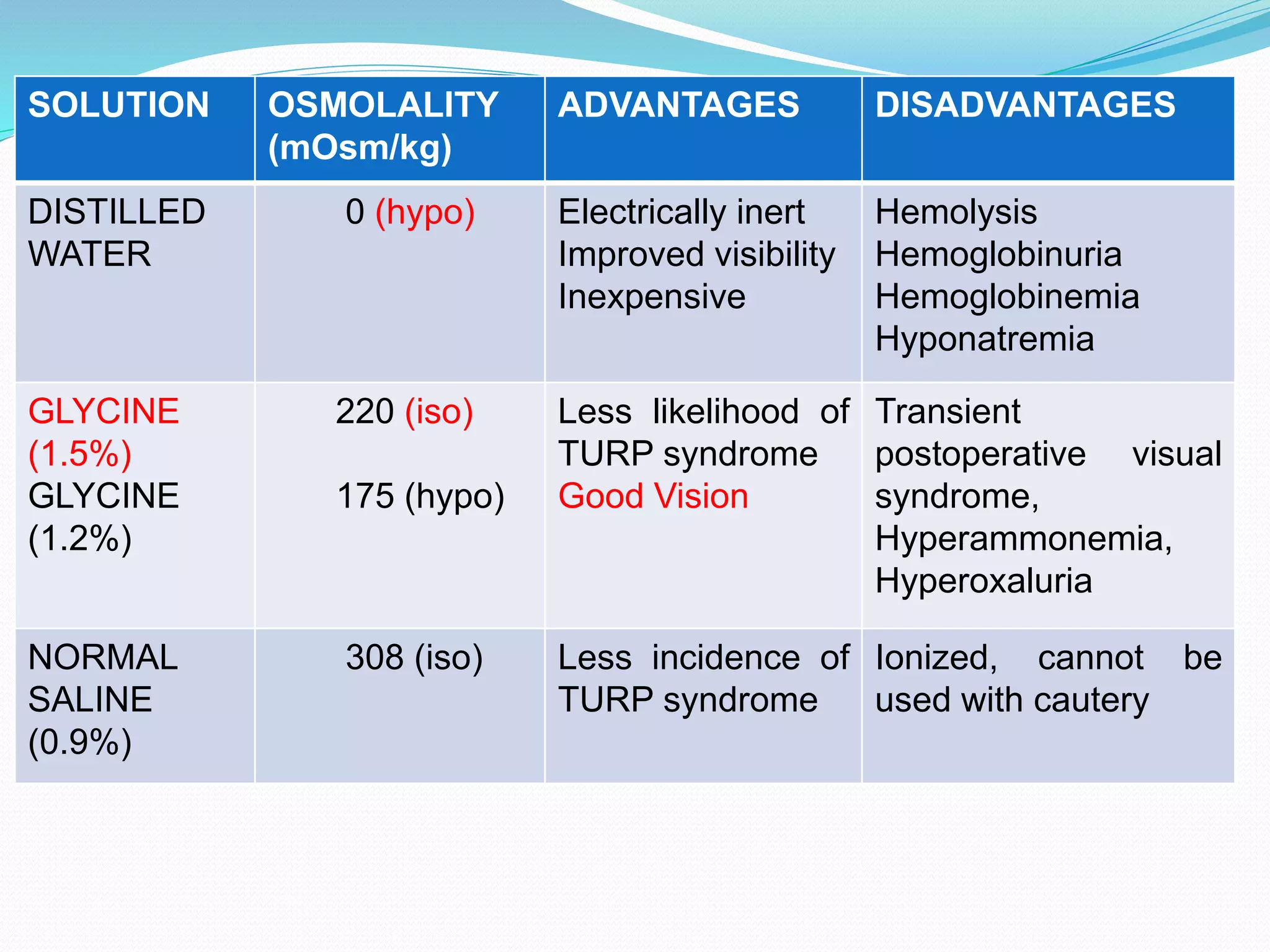
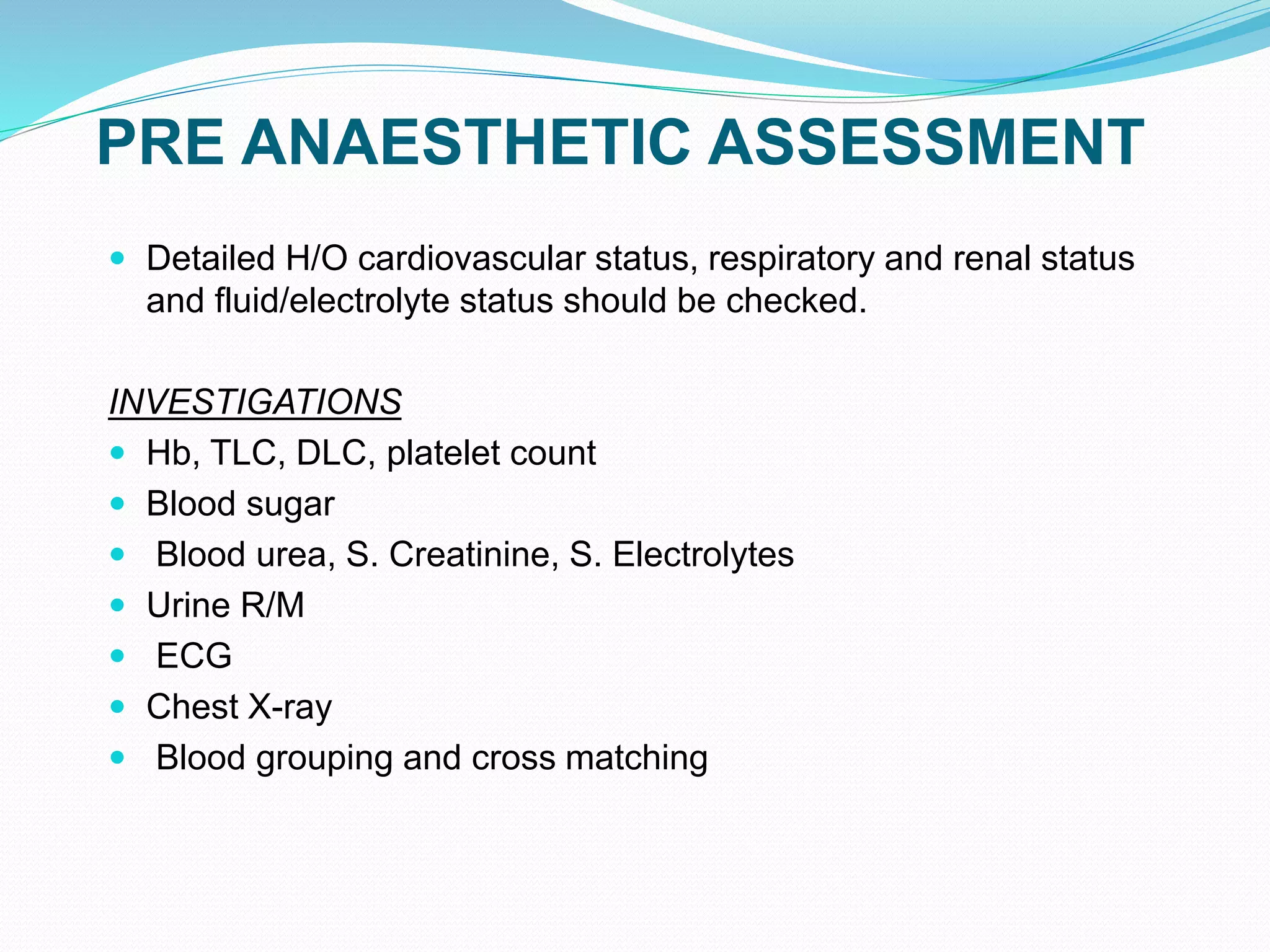
The document provides information on the anatomy, microscopic anatomy, blood supply, nerve supply, and common conditions of the prostate gland such as benign prostatic hyperplasia. It discusses the procedure of transurethral resection of the prostate in detail, including preoperative considerations, choices of anesthesia, intraoperative monitoring, complications such as TURP syndrome, and their prevention and management. TURP syndrome is caused by excessive absorption of irrigating fluids and can lead to hyponatremia, hypervolemia, and other electrolyte abnormalities.



























![TREATMENT
Depends on the detection of hyponatremia – serial sodium
measurements must be done whenever unexplained changes
in BP or cerebral irritation is seen.
Infusion of clear fluids should be suspended.
Blood loss should be replaced by slow blood transfusion.
Loop diuretic – furosemide can be given.
In case of acute hyponatremia with neurological features,
rapid correction till neurological improvement is to be done.
Na deficit = (DESIRED [NA] - CURRENT [NA]) X 0.6 * Bd WT (KG)
(*use 0.6 for men and 0.5 for women).](https://image.slidesharecdn.com/anaesthesiaforturpdr-200224181834/75/Anaesthesia-for-turp-dr-amir-34-2048.jpg)










