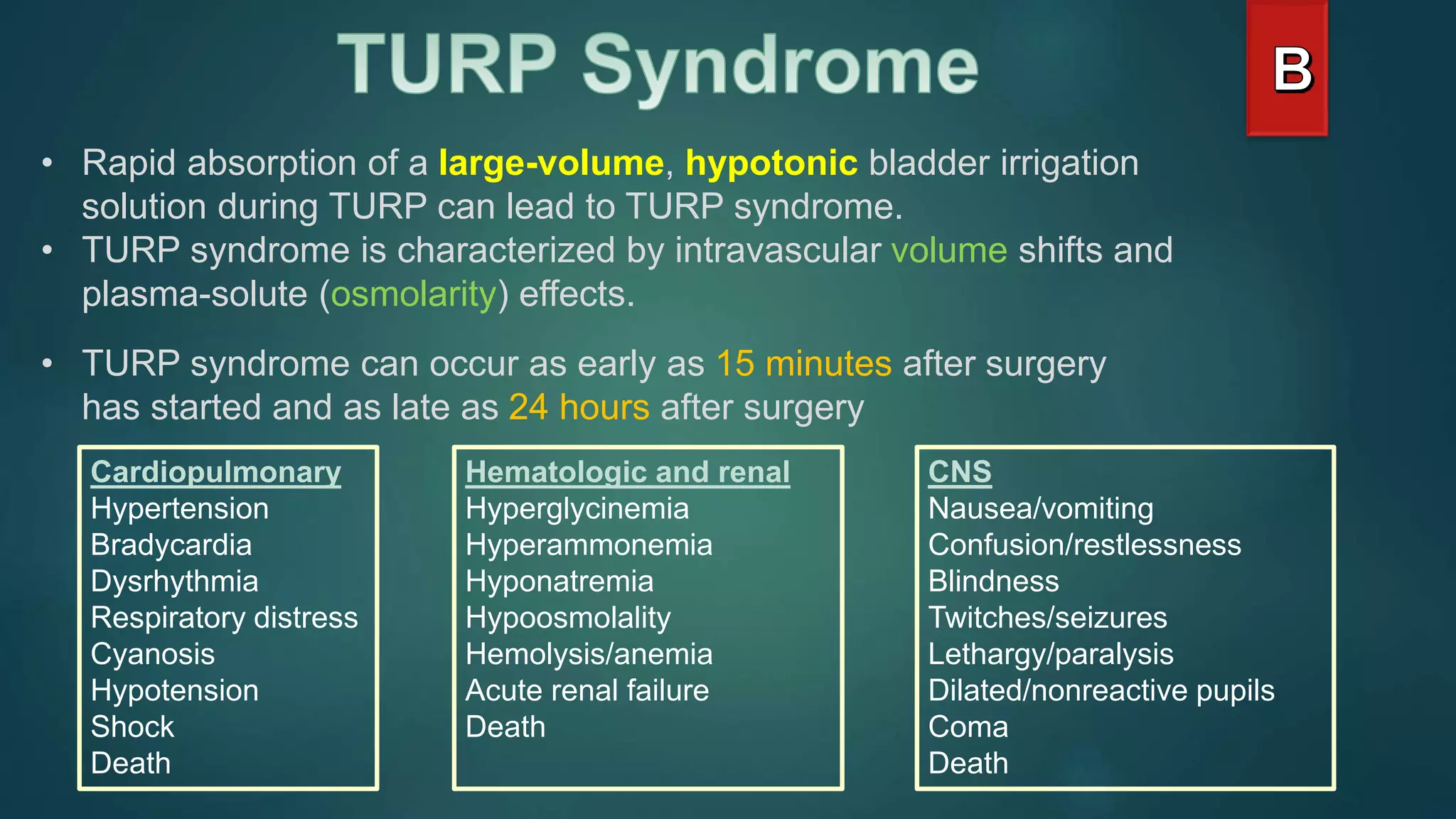
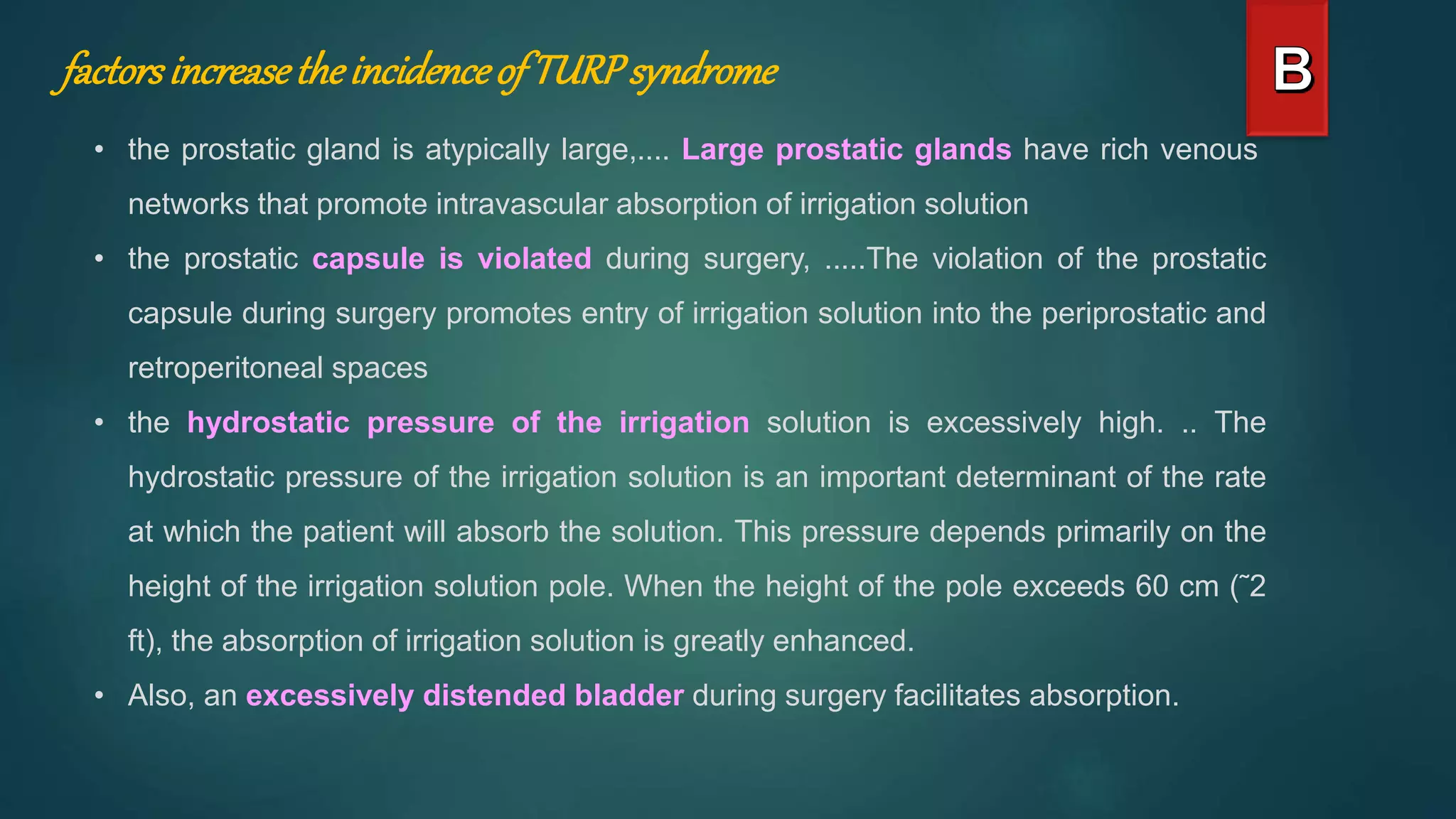
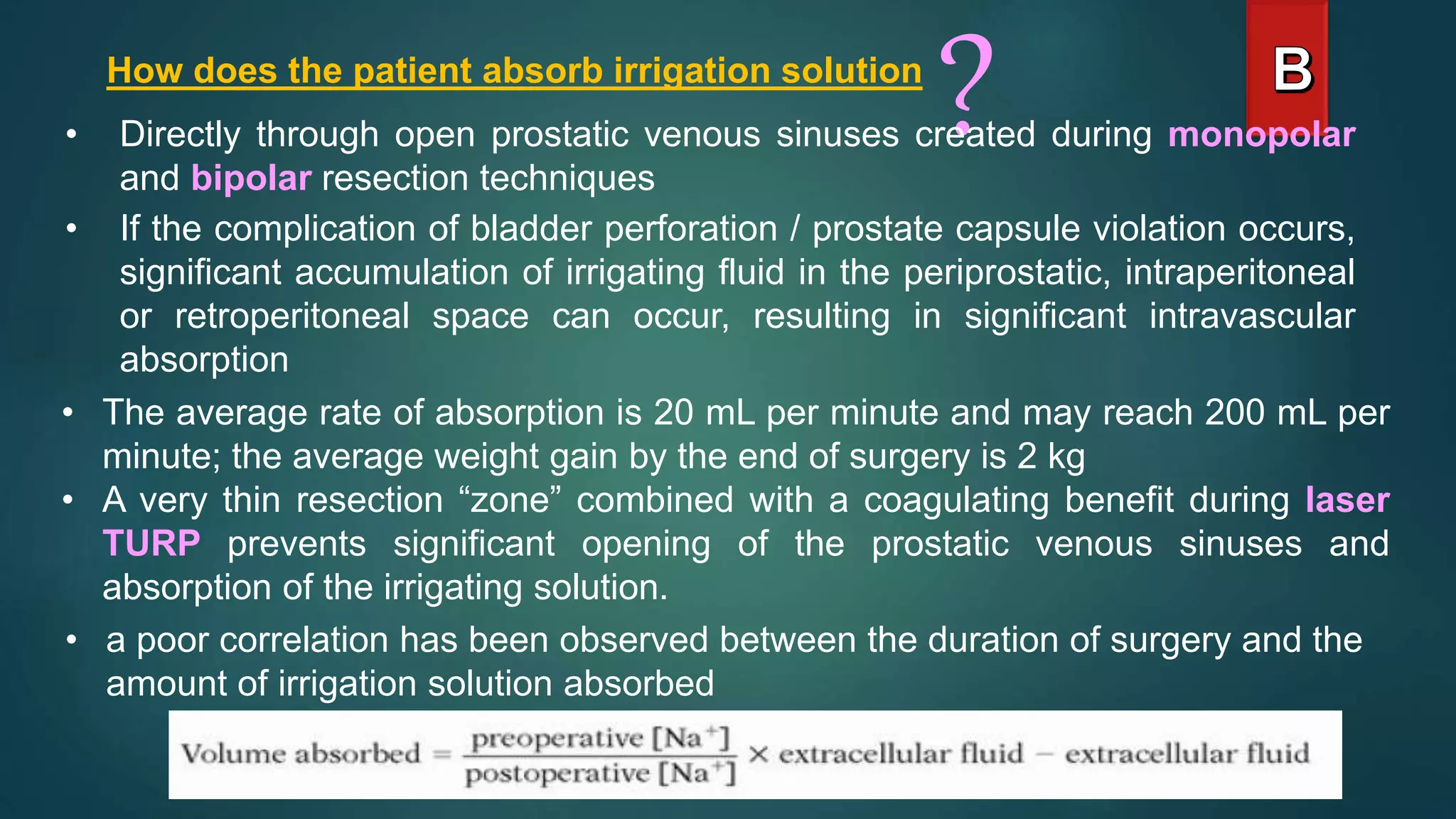
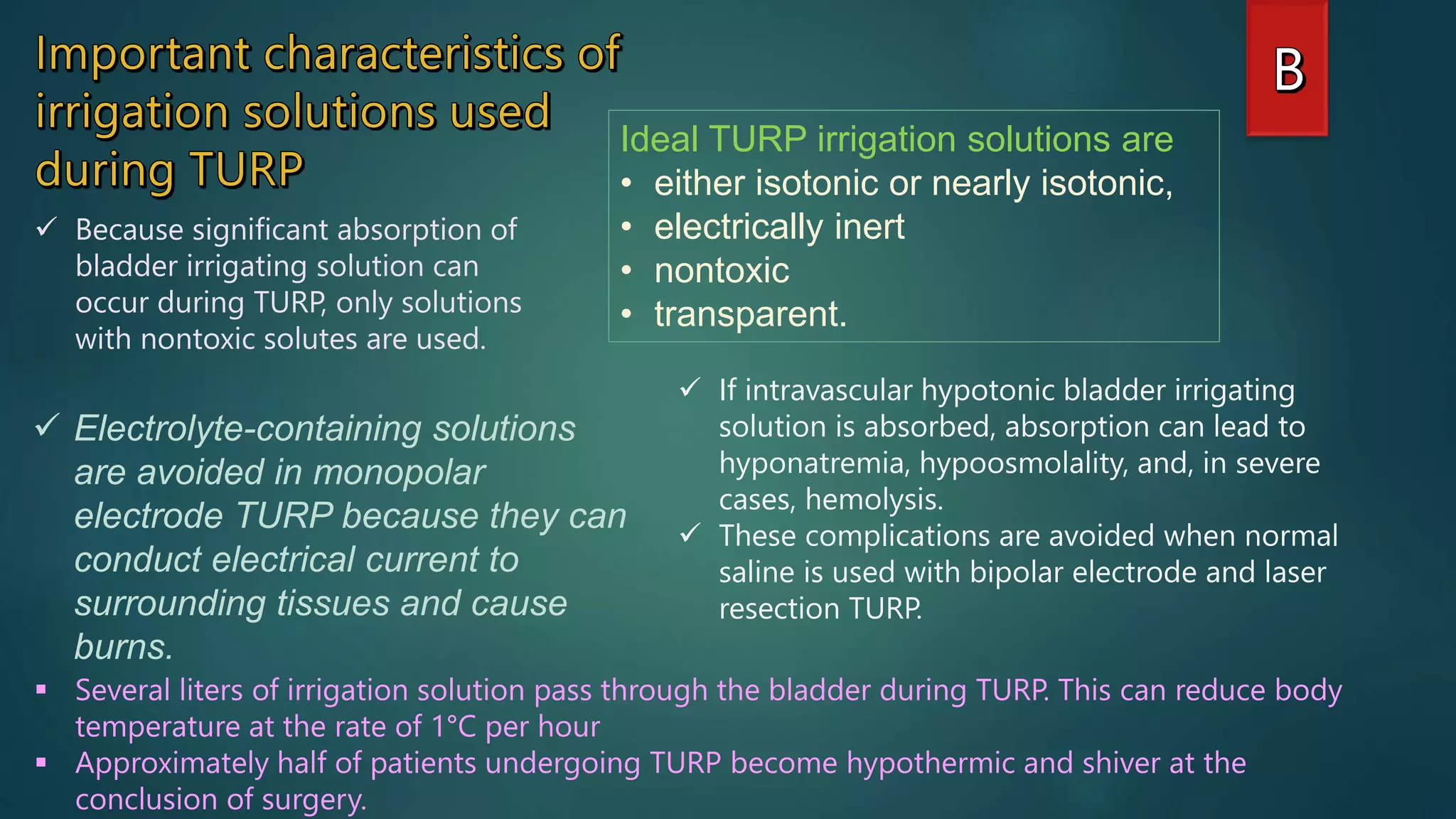
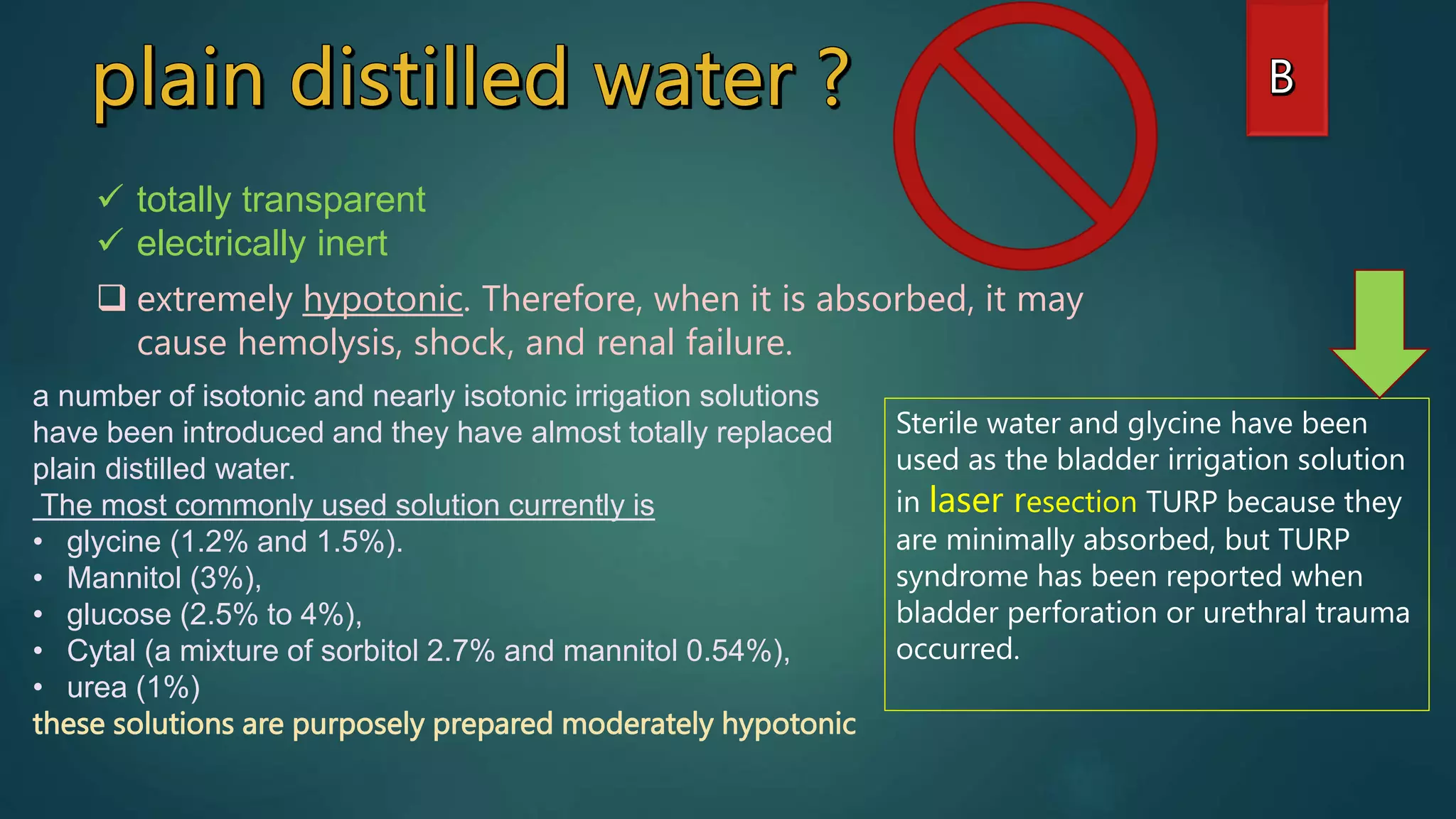
TURP is a common procedure for treating enlarged prostate but it carries risks. Regional anesthesia is preferred to allow early detection of complications like fluid absorption. Irrigation solutions must be nontoxic if absorbed. Complications can include TURP syndrome from fluid shifts, leading to hyponatremia, seizures, or pulmonary edema. Treatment involves terminating surgery, diuresis, oxygen, and correcting electrolyte imbalances with hypertonic saline if needed.