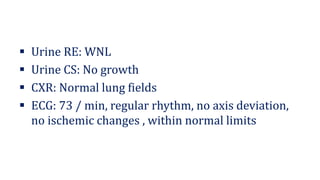
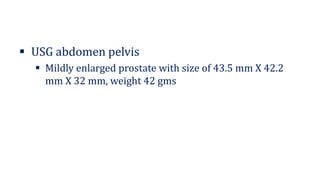
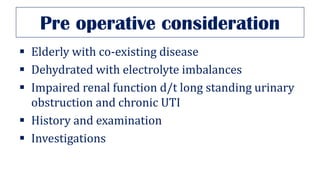
1. A 58-year-old male presented with increased urinary frequency and difficulty passing urine for the past 6 months. Examination found an enlarged prostate and ultrasound revealed a prostate size of 43.5 x 42.2 x 32 mm.
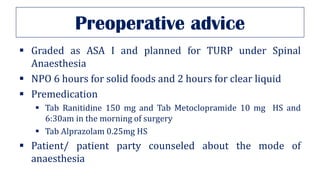
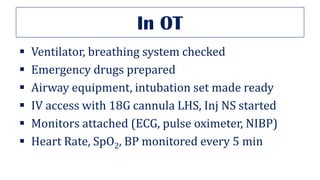
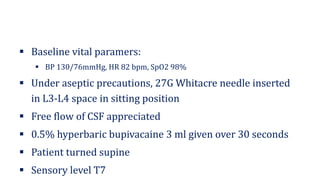
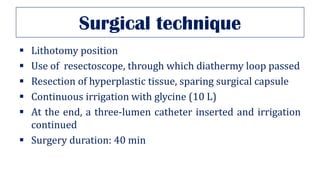
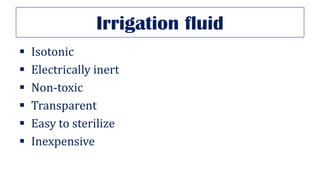
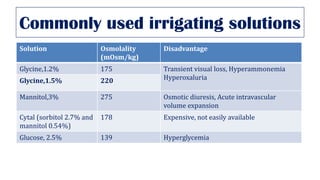
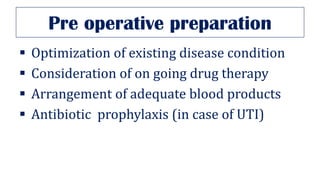
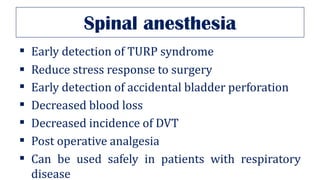
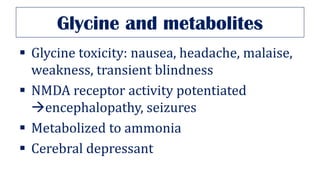
2. The patient underwent a transurethral resection of the prostate (TURP) under spinal anesthesia. The procedure took 40 minutes with irrigation using glycine solution.
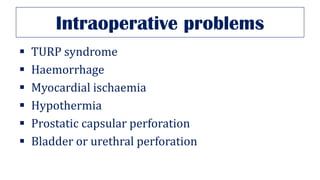
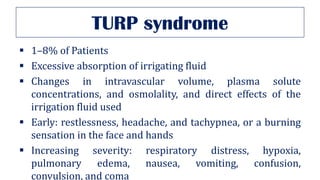
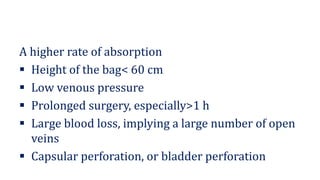
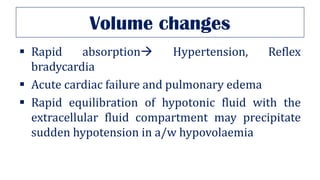
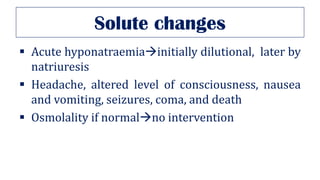
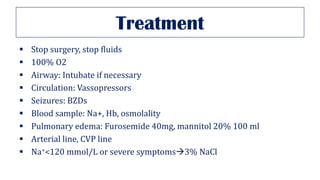
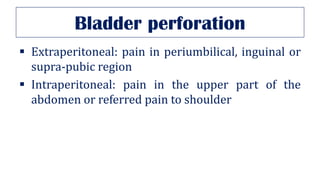
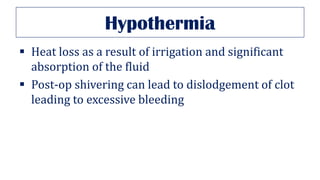
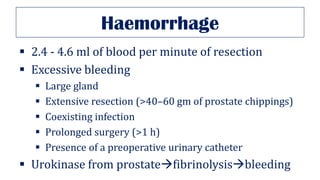
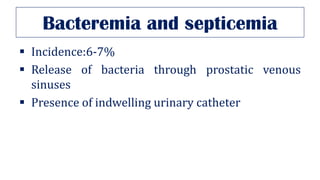
3. Complications of TURP include TURP syndrome from excessive fluid absorption, hemorrhage, hypothermia, bladder or urethral perforation. Care must be taken to prevent high irrigation pressures and prolonged procedures to reduce risks.