This document discusses anaesthesia considerations for emergency laparotomy in critically ill patients. Key points include:
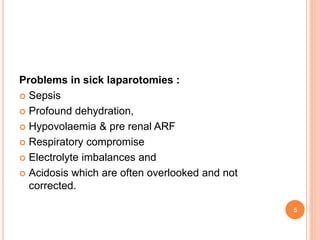
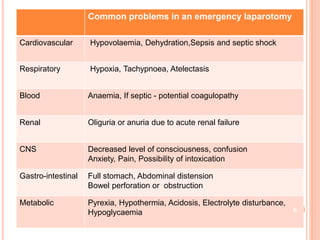
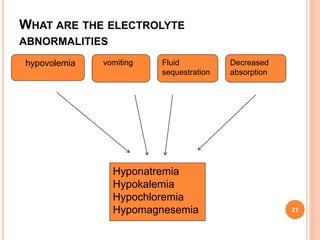
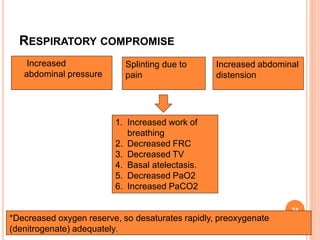
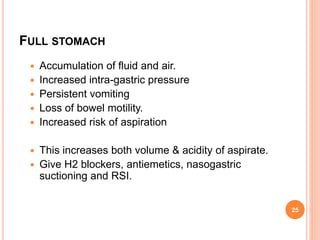
- Patients often present late with sepsis, dehydration, electrolyte imbalances, and respiratory compromise from abdominal issues.
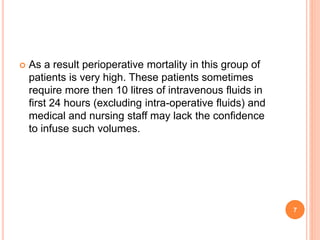
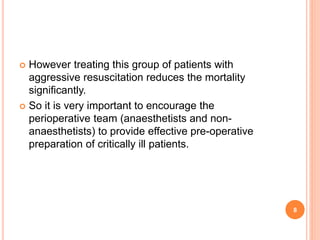
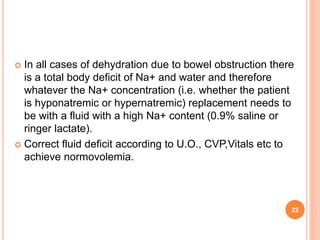
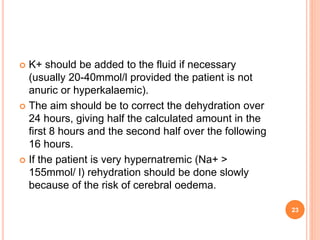
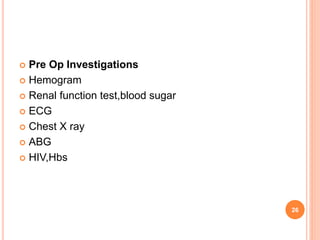
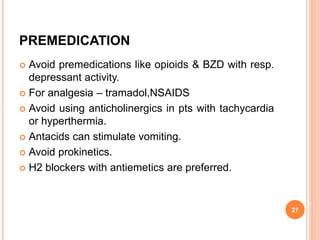
- Preoperative resuscitation is important to optimize the patient's condition through fluid resuscitation and correction of acidosis and electrolyte abnormalities over 2-4 hours.
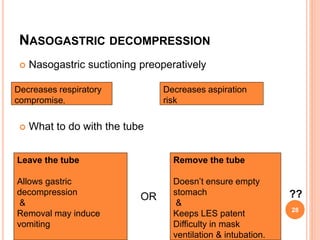
- During resuscitation, airway and breathing are prioritized through oxygen supplementation. Circulation is addressed through IV access and fluid administration while monitoring urine output and electrolytes.
- Full preoperative optimization improves outcomes, but delays before surgery should be avoided in septic patients where early surgical management is beneficial