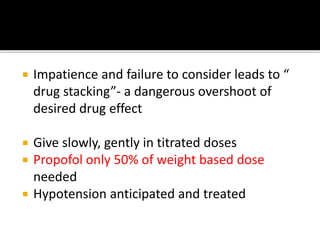
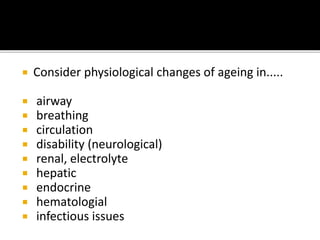
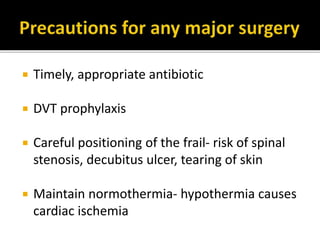
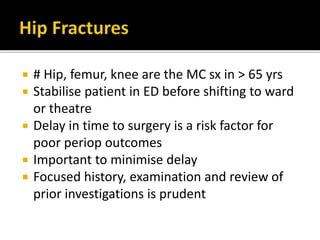
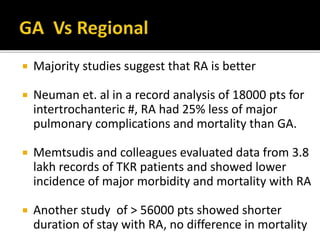
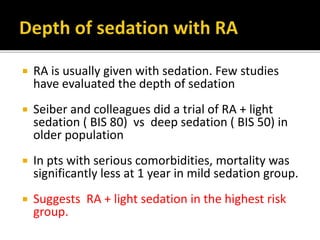
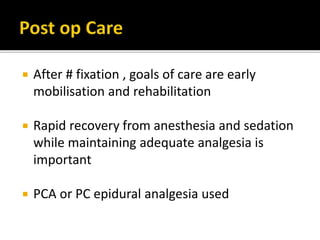
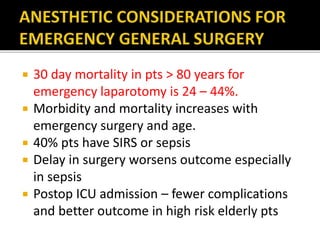
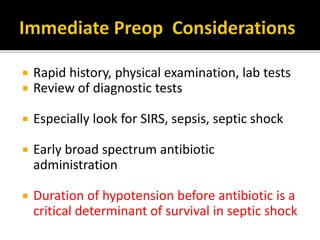
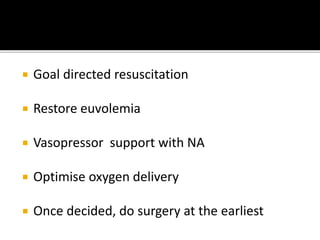
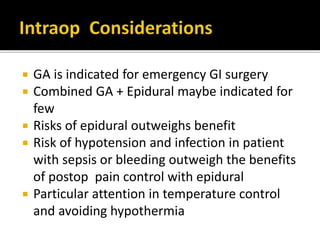
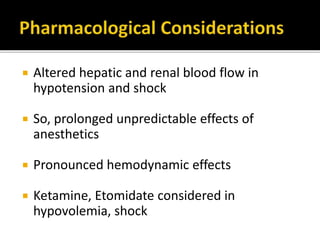
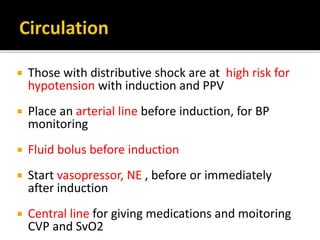
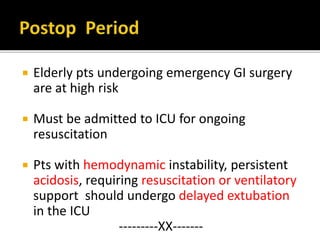
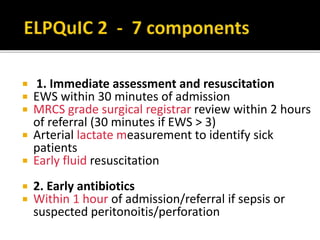
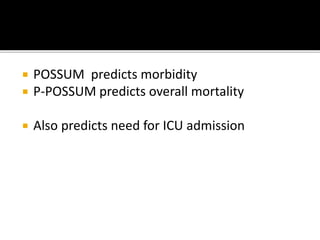
This document summarizes key considerations for anesthesia management in elderly patients undergoing emergency surgery. It recommends preoperative optimization, careful titration of anesthetic drugs due to increased sensitivity in elderly, and goal-directed resuscitation for patients presenting with abdominal emergencies. Regional anesthesia is preferred over general anesthesia for hip surgeries when possible. Close postoperative monitoring in the ICU is important for high-risk elderly patients after emergency laparotomy to improve outcomes.
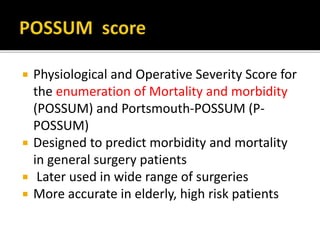
![ Values calculated by simple mobile apps
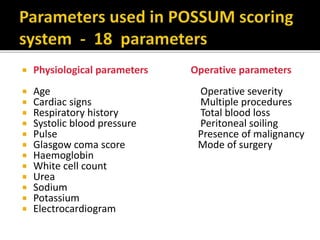
Each of the 18 factors, which are weighted to a value of 1,
2, 4 ,8 depending on measured variables
Predicted POSSUM mortality
ln [R/(1−R) = −7.04 + 0. 13 × physiological score
+ 0.16 x operative score
where R is the predicted mortality score.
Predicted P-POSSUM mortality
ln [R/(1−R)] = −9.37 + 0.19 × physiological
score + 0.15 x operative score](https://image.slidesharecdn.com/reviewarticlethalaparotomygeriatric-180501074756/85/Geriatric-Anaesthesia-39-320.jpg)
