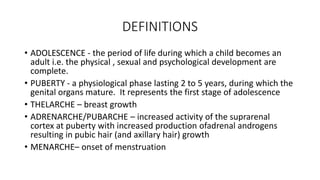
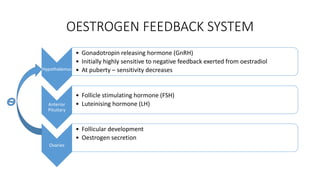
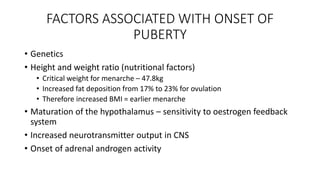
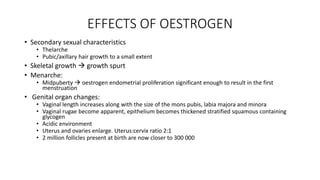
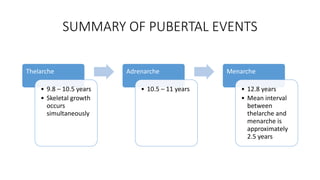
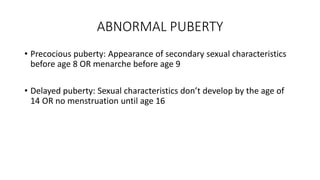
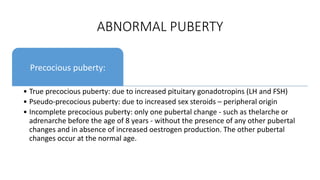
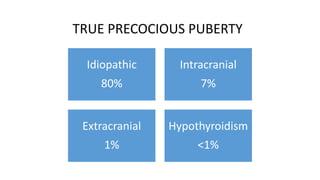
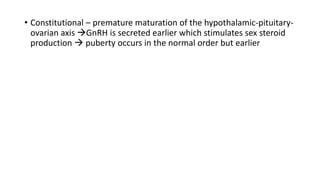
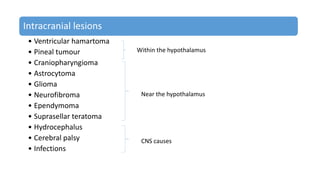
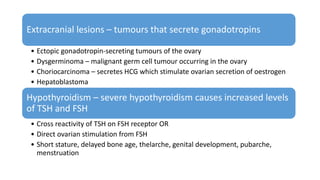
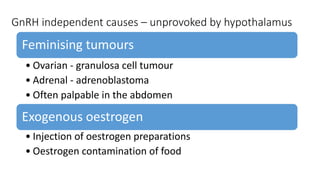
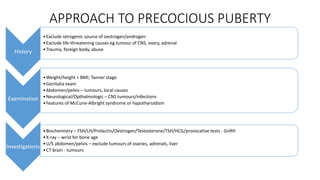
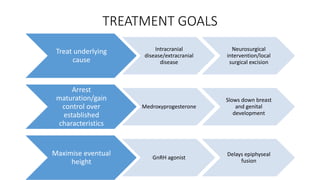
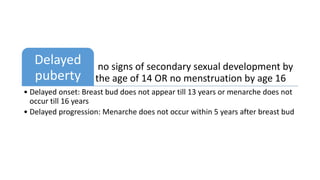
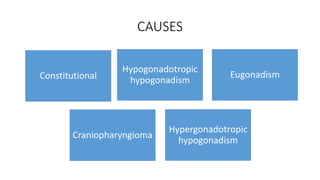
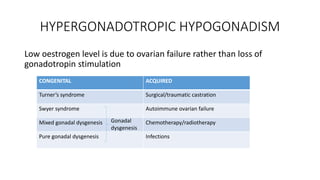
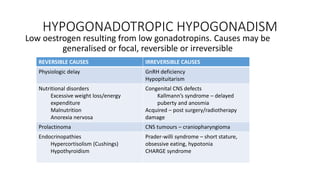
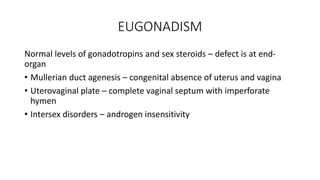
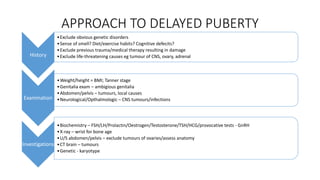
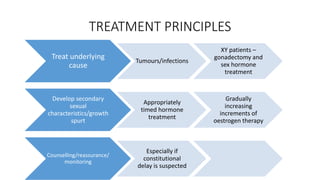
This document discusses normal and abnormal puberty. It begins by defining key terms like adolescence and puberty. It then outlines the normal sequence of pubertal events including thelarche, adrenarche, and menarche. It also discusses factors that influence the onset of puberty. Abnormal puberty is categorized as either precocious or delayed. Precocious puberty can be true, pseudo, or incomplete. Causes and treatment approaches are provided. Delayed puberty can be caused by hypergonadotropic hypogonadism, hypogonadotropic hypogonadism, or eugonadism. The document concludes with discussing the approach to evaluating and treating delayed puberty.