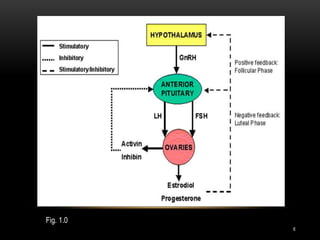
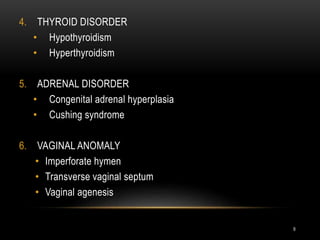
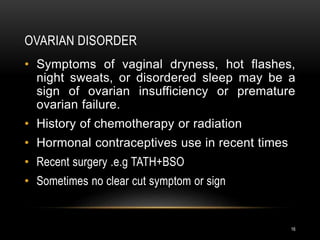
This document provides an overview of amenorrhea, beginning with definitions and classifications of primary and secondary amenorrhea. It then discusses the pathophysiology of the hypothalamic-pituitary-ovarian axis and menstrual cycle. The main causes of amenorrhea are outlined, including physiological causes as well as disorders of the hypothalamus, pituitary, thyroid, adrenals, ovaries, and uterus. The document describes the clinical evaluation of amenorrheic patients, including taking a thorough medical history and conducting a physical exam and laboratory investigations. Finally, medical and surgical treatment options are presented depending on the underlying cause of the amenorrhea.