The document discusses the altered-cast technique for fabricating removable partial dentures (RPDs). Key points include:
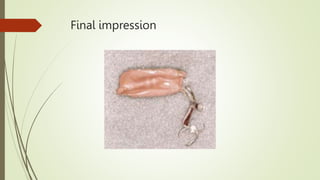
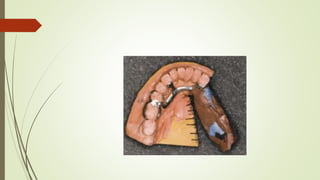
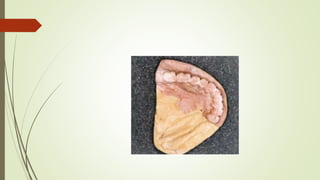
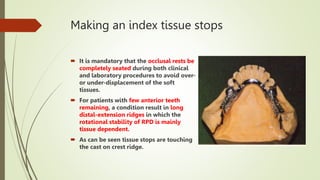
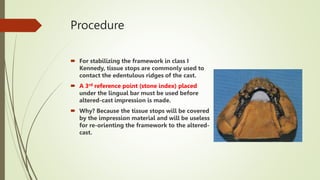
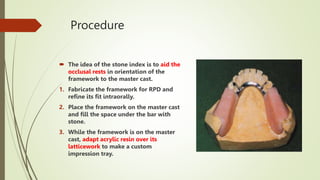
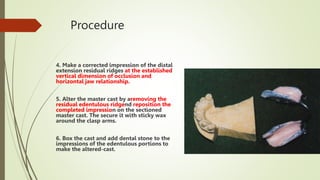
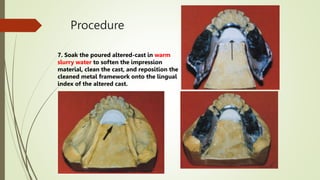
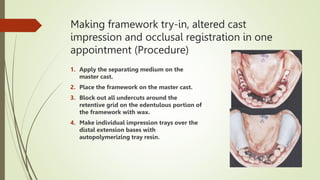
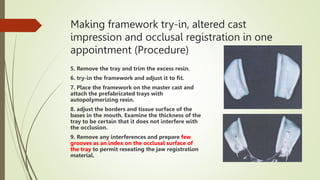
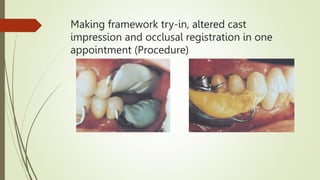
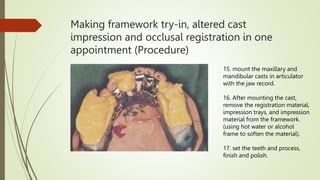
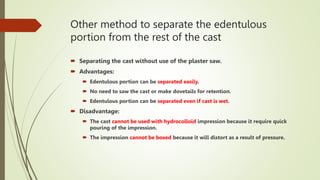
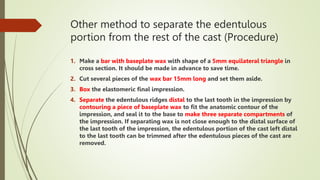
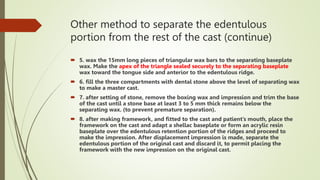
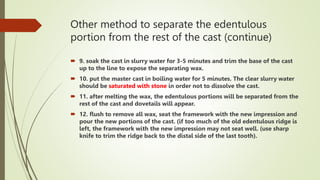
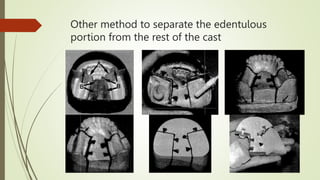
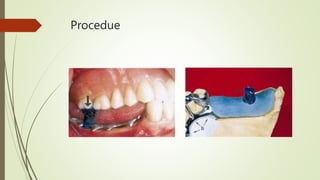
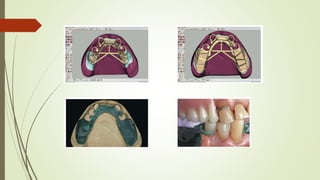
- The altered-cast technique involves making an impression of the residual ridges in their functional position after fitting the RPD framework, then separating the edentulous portion of the master cast to reposition it based on the new impression.
- This technique aims to improve the fit of the RPD base to the residual ridges and reduce stress on abutment teeth.
- The procedure involves border molding a custom tray attached to the fitted framework, then making an impression using elastic materials like polysulfide.
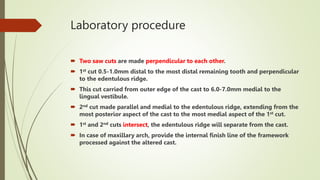
- In the lab, the edentulous portion of the master cast is