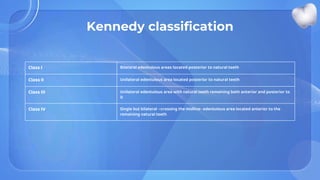
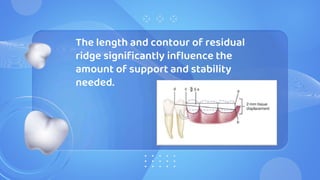
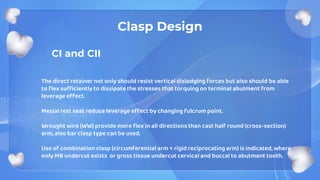
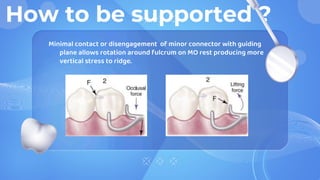
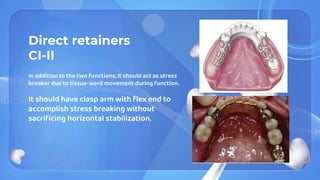
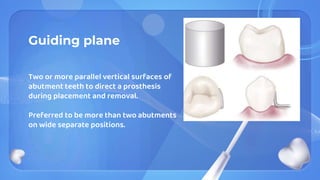
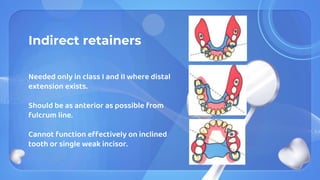
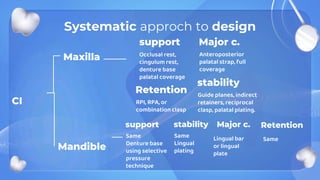
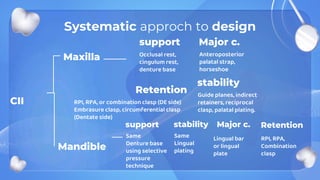
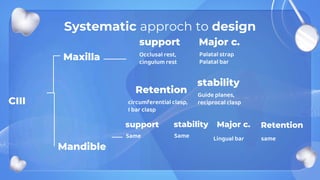
This document discusses principles of removable partial denture (RPD) design, including Kennedy classification systems for different clinical situations, considerations for support and retention, and a systematic approach to RPD design. Key points covered include differentiating tooth-supported versus tissue-supported designs, using minor connectors along guiding planes for optimal stress distribution, and employing techniques like indirect retainers and reciprocal clasps to restrict horizontal movement. The summary concludes that RPD design should be systematically developed based on factors like the location of support and how retention is achieved.