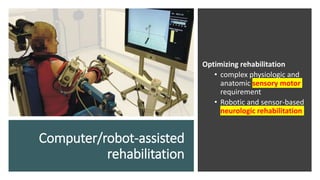
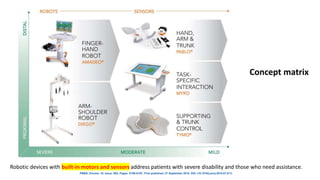
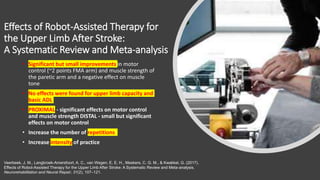
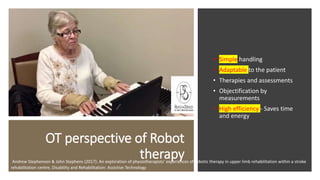
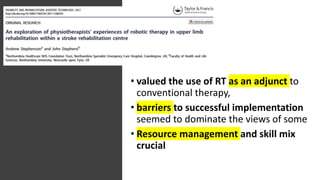
Robot-assisted therapy is an effective adjunct to conventional upper limb rehabilitation after stroke. Robotic devices can provide intensive, repetitive, interactive therapy and allow accurate assessment of motor control and strength. Well-designed robots optimize rehabilitation by addressing complex sensory and motor requirements through varied, motivating activities and feedback. When combined with therapists, robots may improve outcomes, increase therapy intensity and efficiency, and help address workforce shortages in rehabilitation clinics.