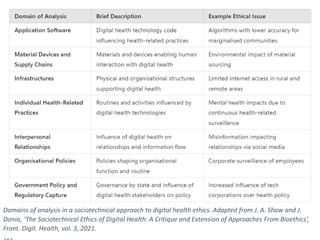
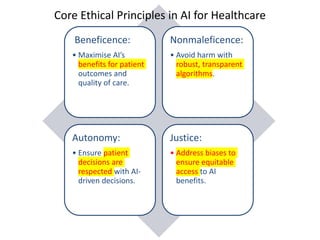
The document discusses the ethical implications of generative AI in healthcare, emphasizing core principles such as beneficence, nonmaleficence, autonomy, and justice. It highlights the challenges posed by AI in shared decision-making between patients and physicians and the need for robust governance and ethical frameworks to ensure equitable and responsible AI use. Further, it addresses the complexities of integrating AI in clinical settings, advocating for continuous dialogue among stakeholders to navigate ethical dilemmas effectively.


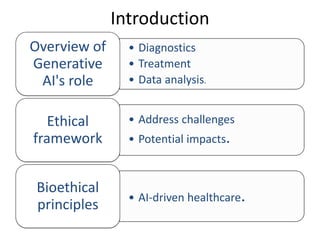


![Short description of
the components of
shared decision-
making
Expanded descriptions of the
components of what is required of
doctors in shared decision-making.
These can be perceived as minimum
standards
How AI can undermine the conditions for shared
decision-making
(a) Understanding
the patient’s
condition
Doctors must understand the
connection between patients’
conditions and the need for potential
interventions on a general, technical,
and normative level and translate them
into individual patients' particular
contexts.
If the clinical outcome of A.I. is beyond what doctors are
able to understand themselves, their clinical
competence is undermined, and by that, a crucial
presupposition for why the patients have reason to
trust them in the first place [38].
(b) Trust in evidence Doctors must base their decisions on
sources of evidence they trust to ensure
the information is relevant and
adequate.
If doctors suggest treatments on the basis of AI sources
to information they cannot fully account for, they force
patients to place blind trust in their recommendations.
This is just another version of paternalism.
(c) Due assessment
of benefits and risks
Doctors must understand all relevant
information of benefits and risks and
trade-offs between them.
If doctors cannot fully understand how and why A.I. has
reached an outcome, say, the classification of an x-ray,
uncertainty regarding assessments of risks, benefits and
trade-offs will follow. This, in turn, undermines
’patients’ reasons to have confidence in their judgments
as their role as the expert in the relation.
(d) Accommodating
” ’patient’s
understanding,
communication,
and deliberation
Doctors must convey an assessment of risks
and benefits to patients in a clear and
accessible manner, ensure they have
understood the information, and invite them to
share their thoughts and deliberate together
on the matter.
If AI systems make it hard for doctors to understand
how and why they reach their outcomes, they cannot
facilitate patients' understanding. Instead, they will
have to paternalistically require that the patient accept
that the A.I. ‘knows best’.
Rahman, N., Thamotharampillai, T., &
Rajaratnam, V. (2024).](https://image.slidesharecdn.com/ethicsofgenerativeaiinhealthcare-241030034815-3490b1e1/85/Ethics_of_Generative_AI_in_Healthcare-pdf-12-320.jpg)