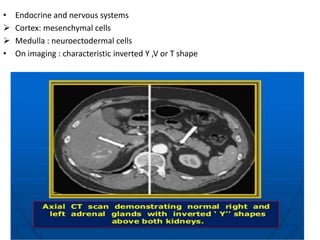
1. Adrenal imaging uses modalities like ultrasound, CT, MRI, and nuclear medicine to evaluate the adrenal glands and detect abnormalities.
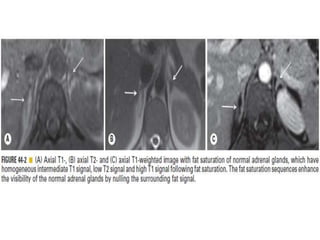
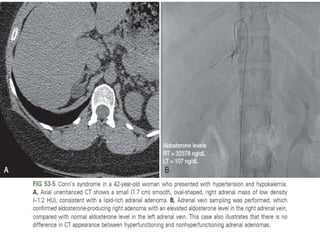
2. CT is often the first choice to evaluate adrenal diseases and can characterize adrenal masses using attenuation values, enhancement patterns, and lipid content analysis.
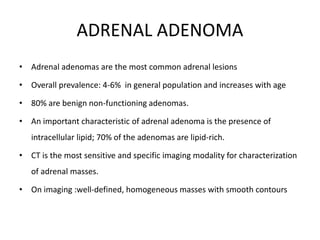
3. Benign adrenal lesions include adenomas, myelolipomas, cysts, infections, and hemorrhages. Adenomas are the most common and often appear well-defined and homogeneous with characteristic lipid content and enhancement patterns on CT and MRI.