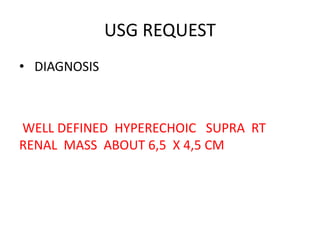
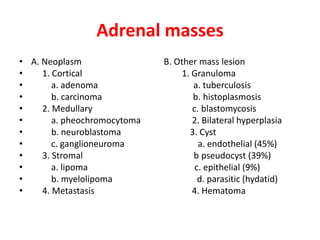
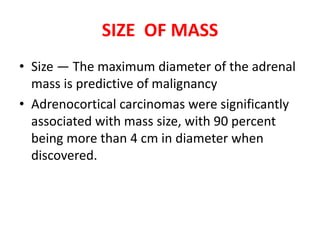
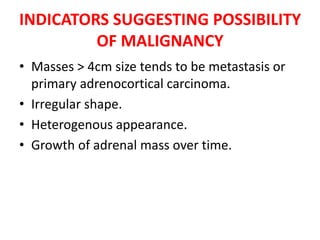
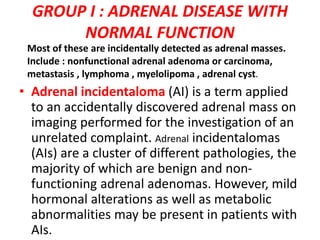
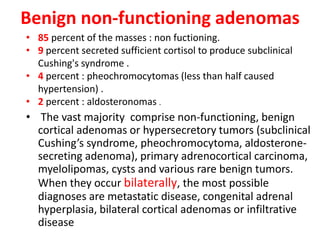
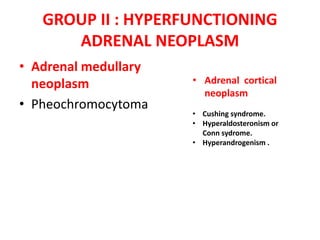
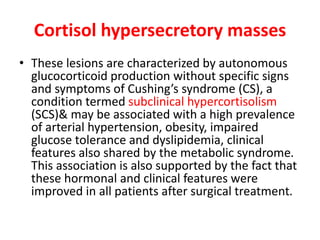
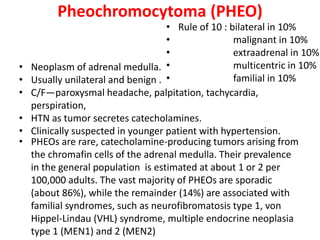
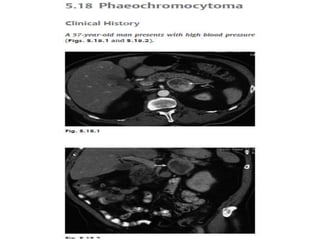
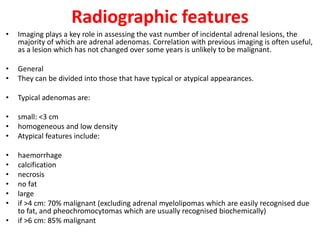
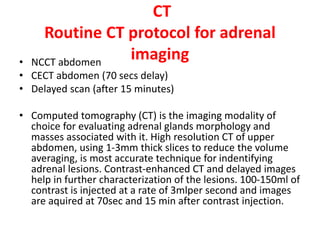
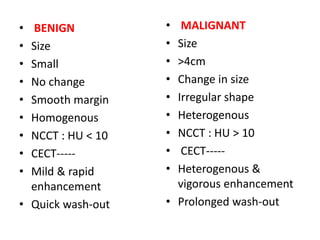
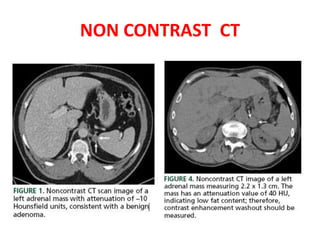
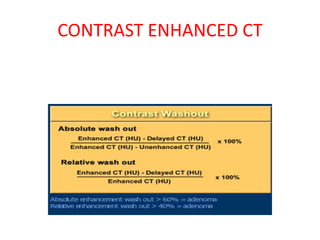
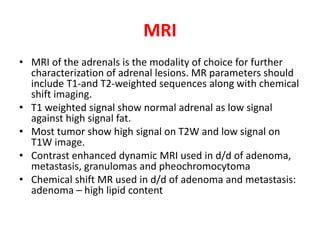
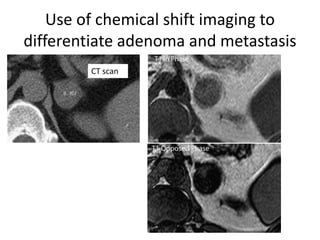
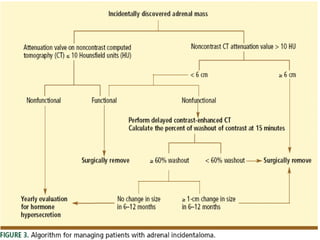
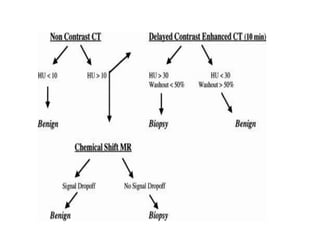
This document discusses the evaluation and diagnosis of an adrenal mass found on imaging. It describes the different types of adrenal masses including benign non-functioning adenomas, hyperfunctioning tumors like pheochromocytomas, metastatic cancers, and adrenal hypofunction. Imaging features on CT and MRI are provided to characterize masses and distinguish benign from malignant lesions based on size, enhancement pattern, chemical shift, and washout characteristics. The majority of incidentally detected adrenal masses are benign non-functioning adenomas.