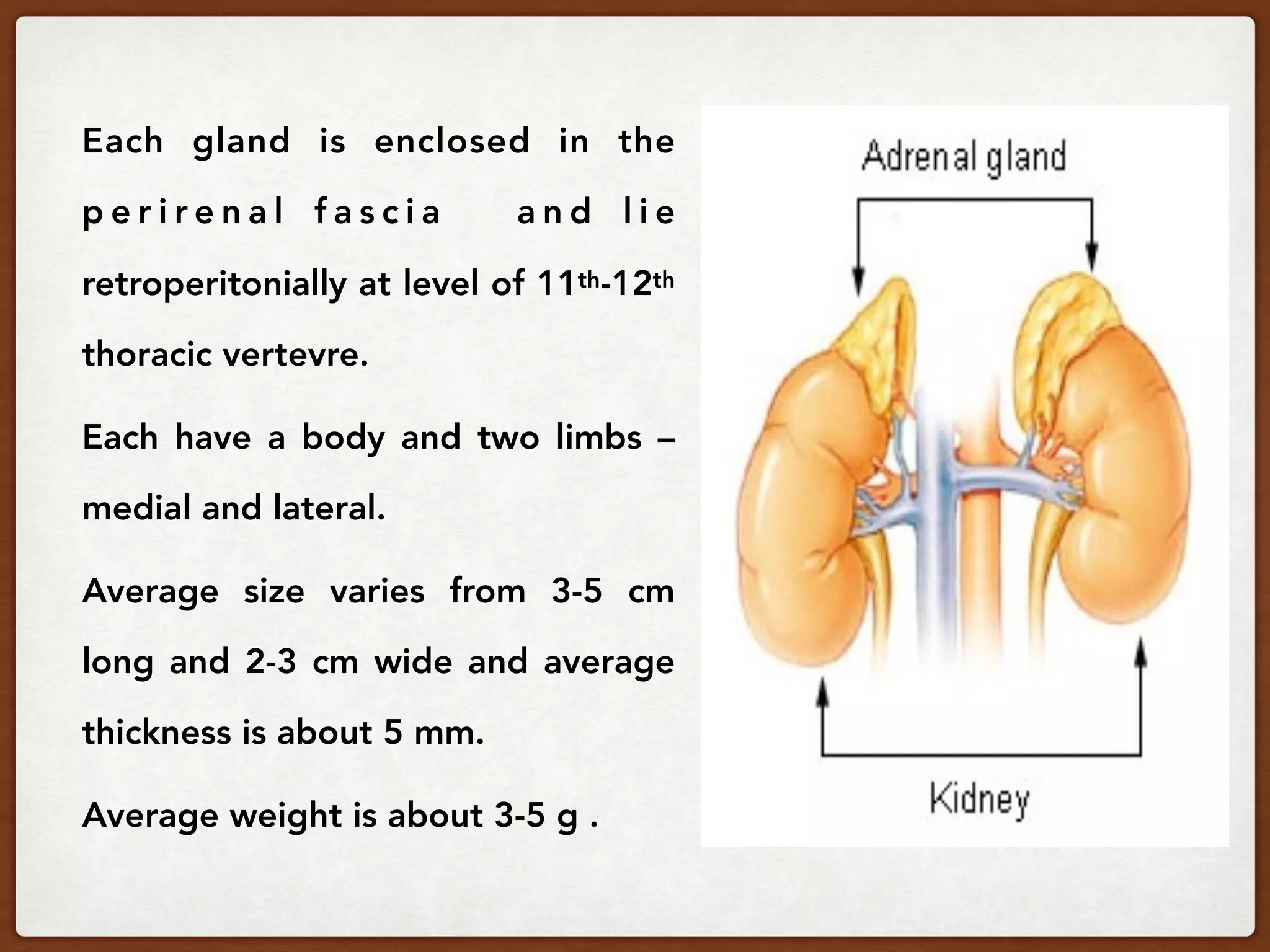
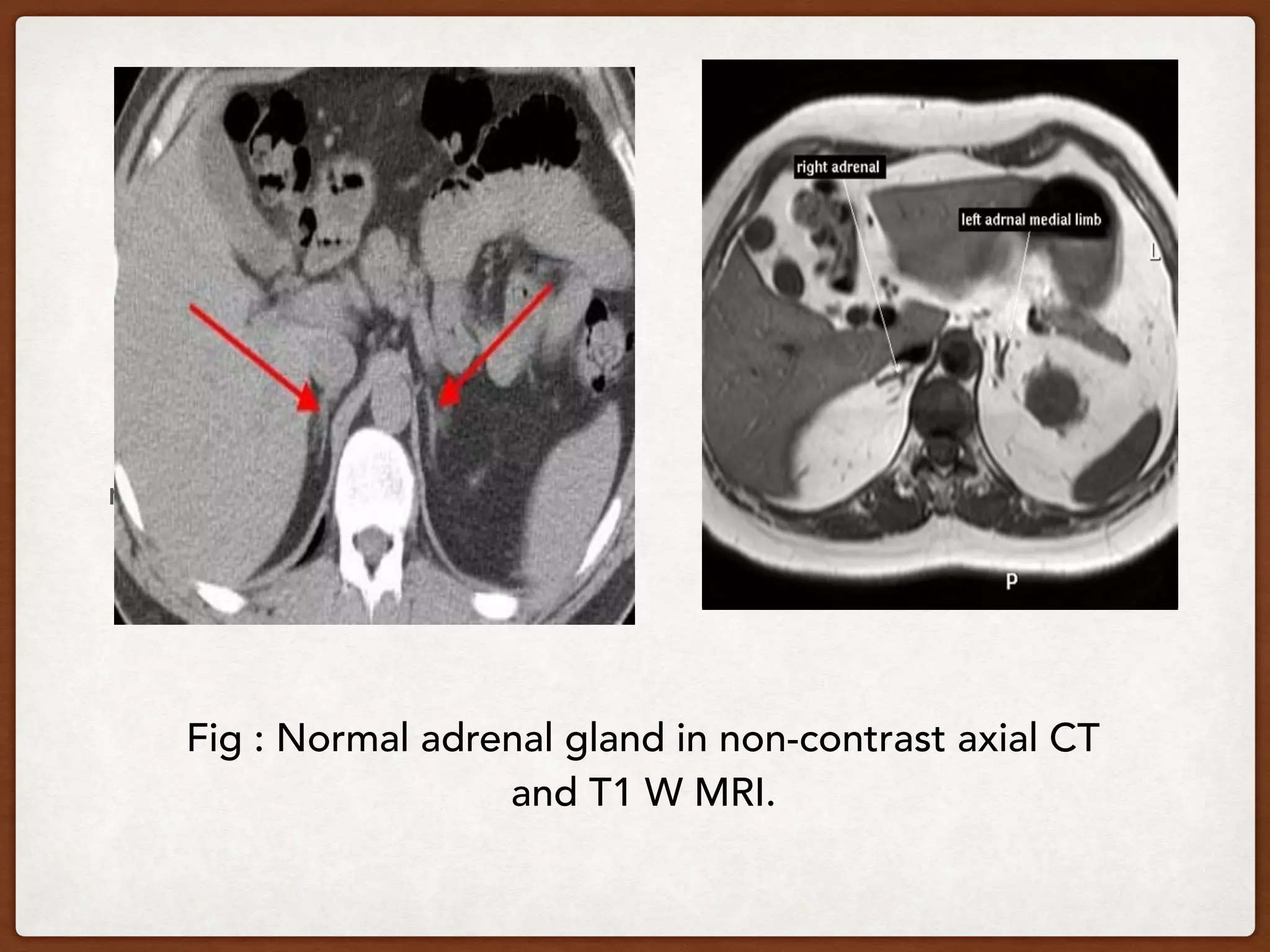
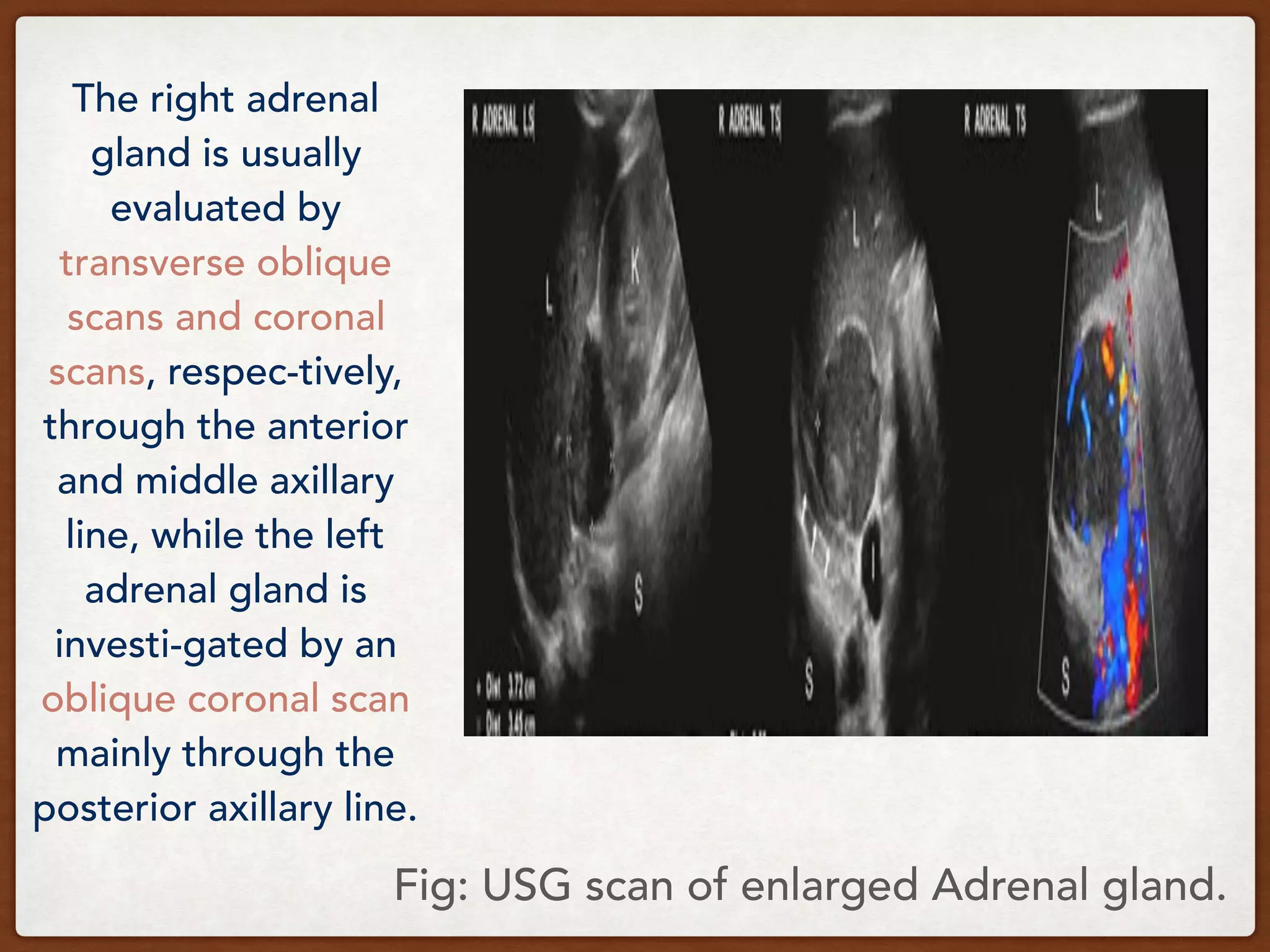
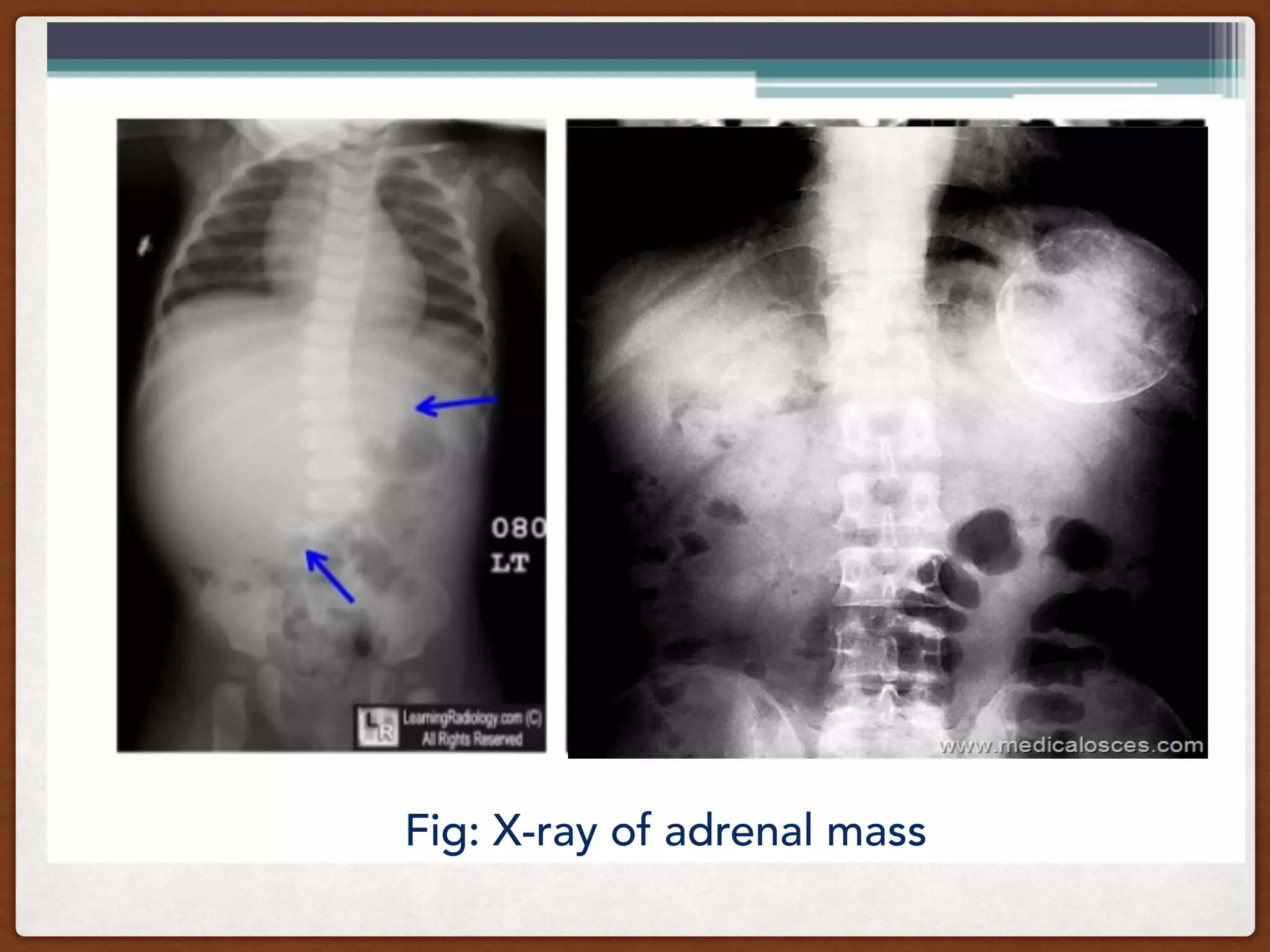
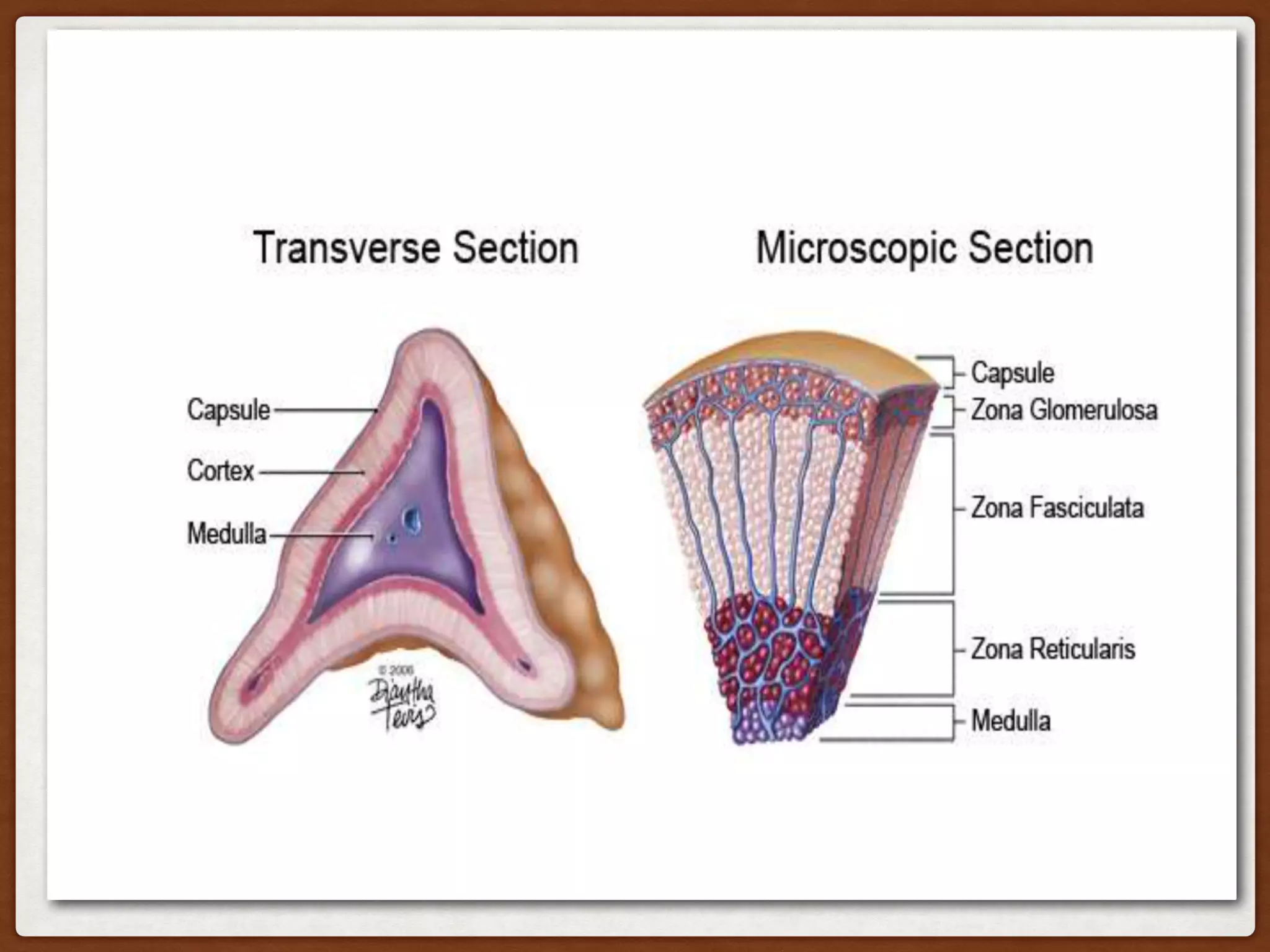
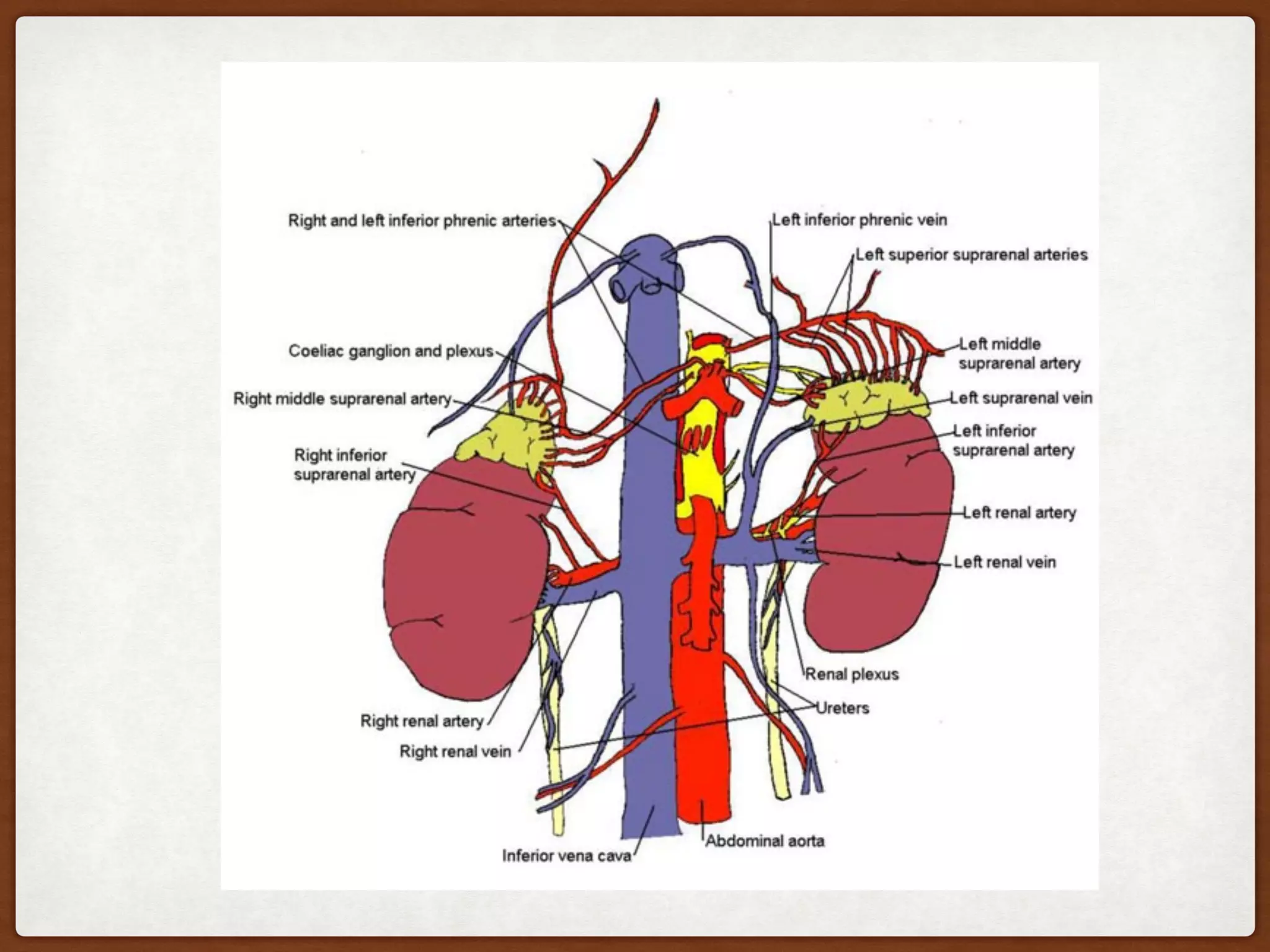
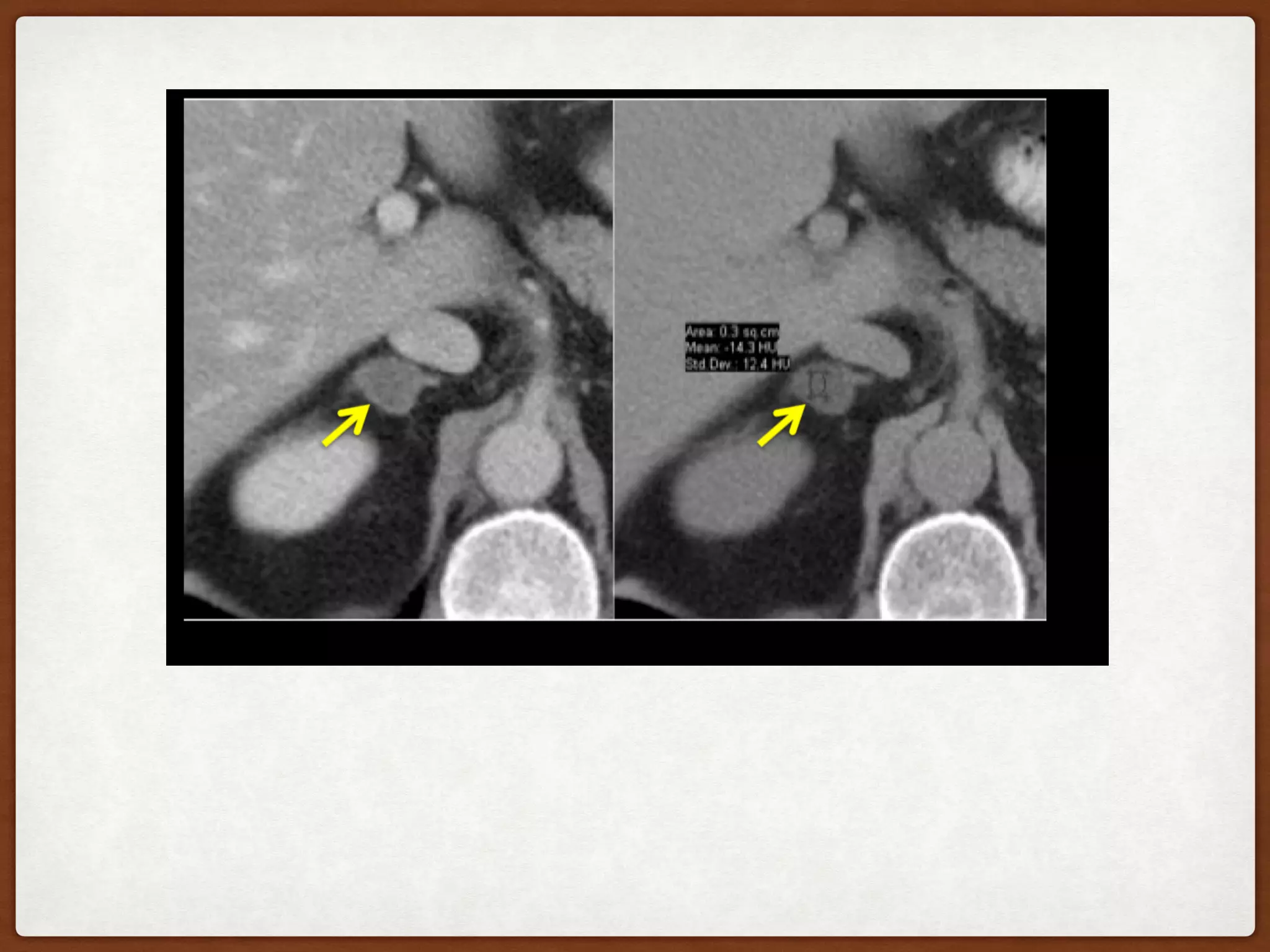
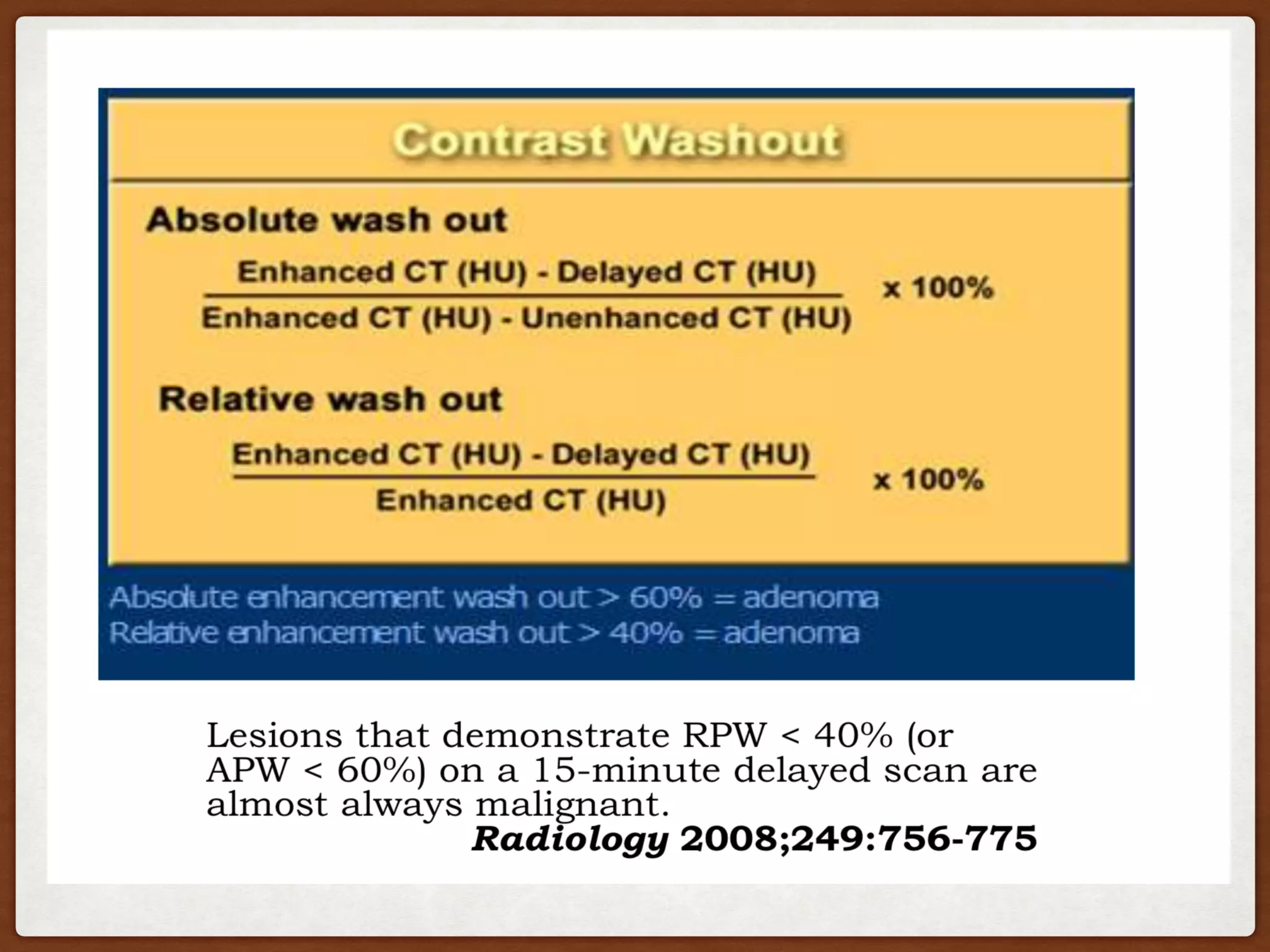
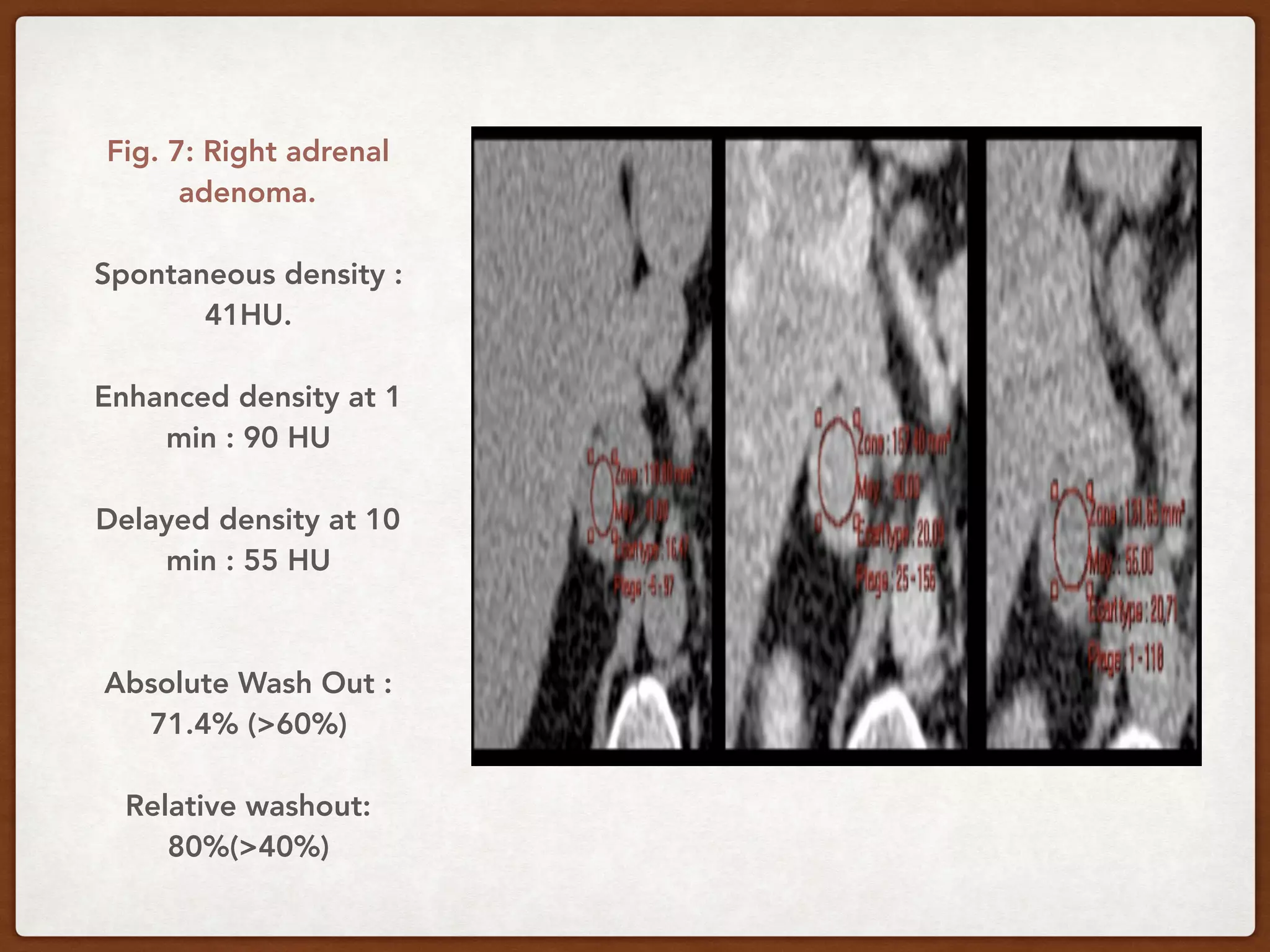
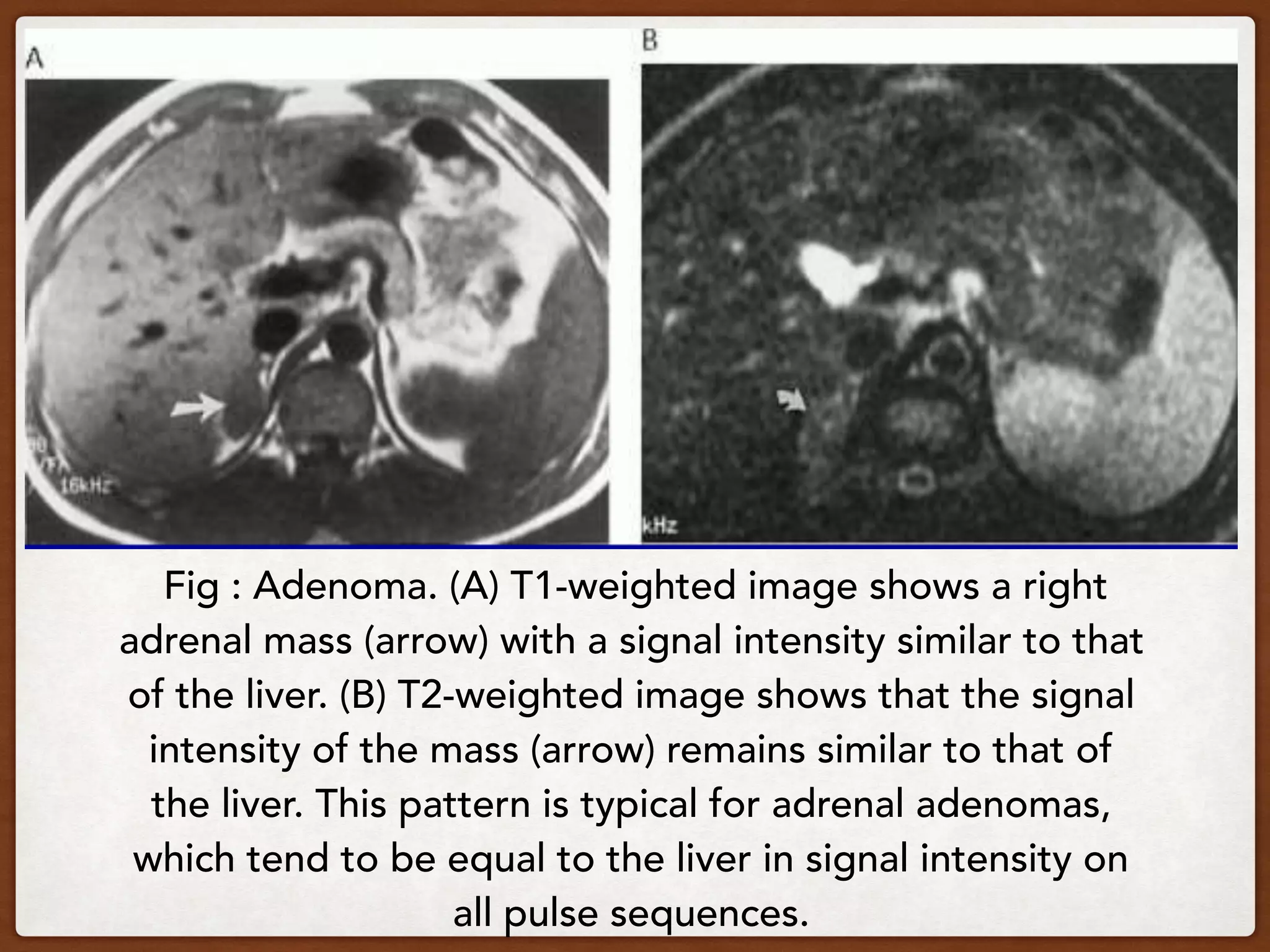
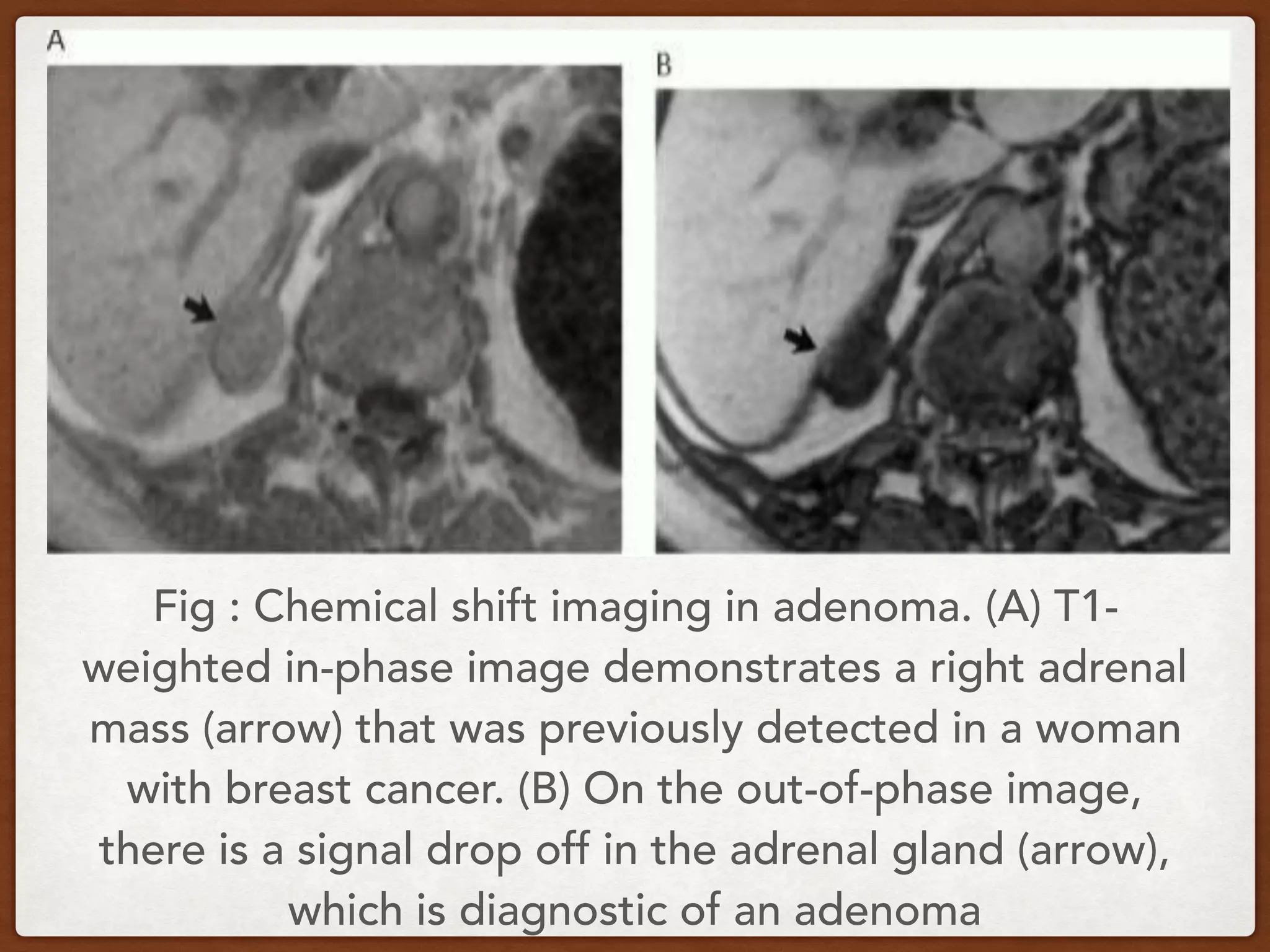
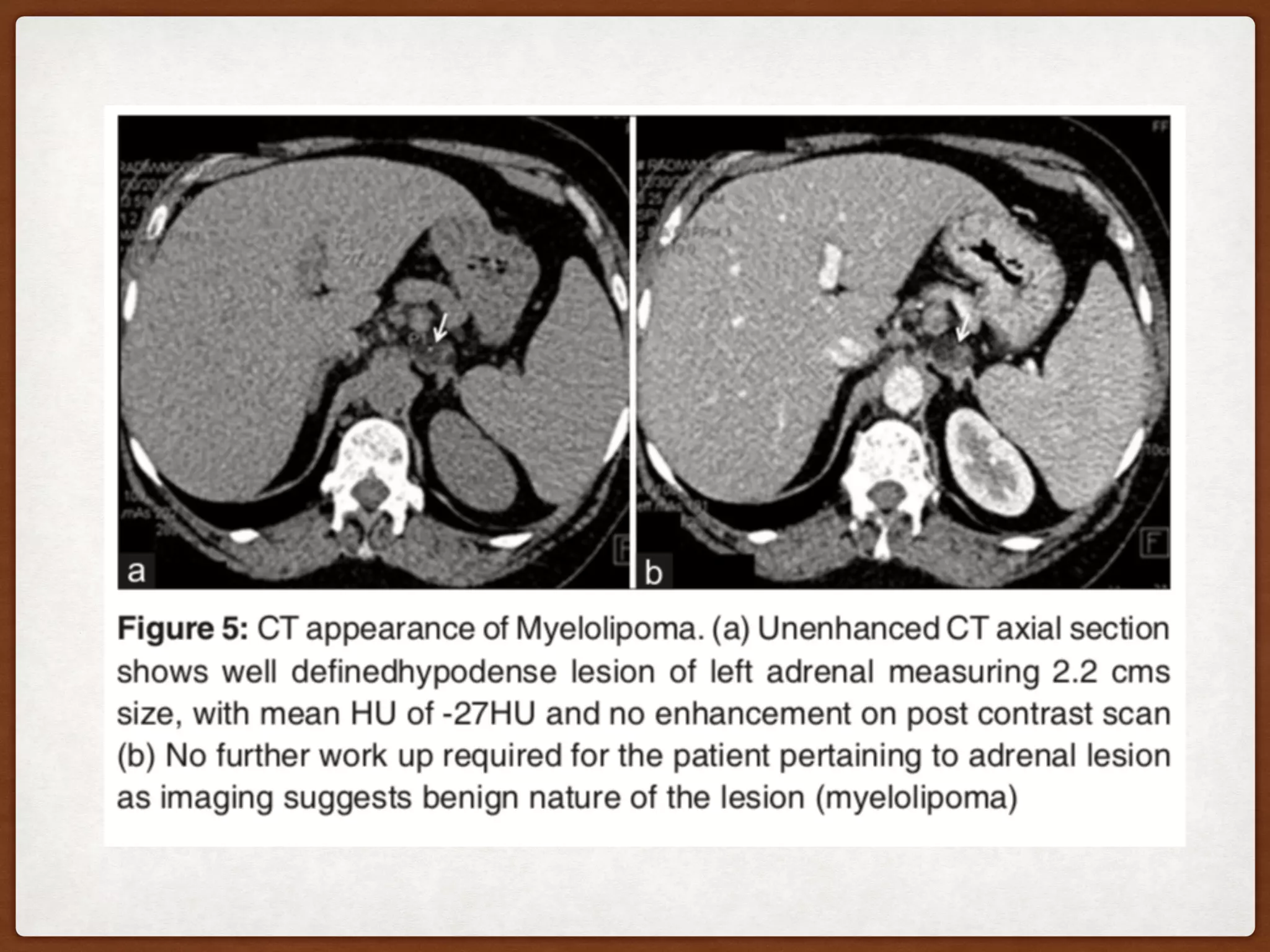
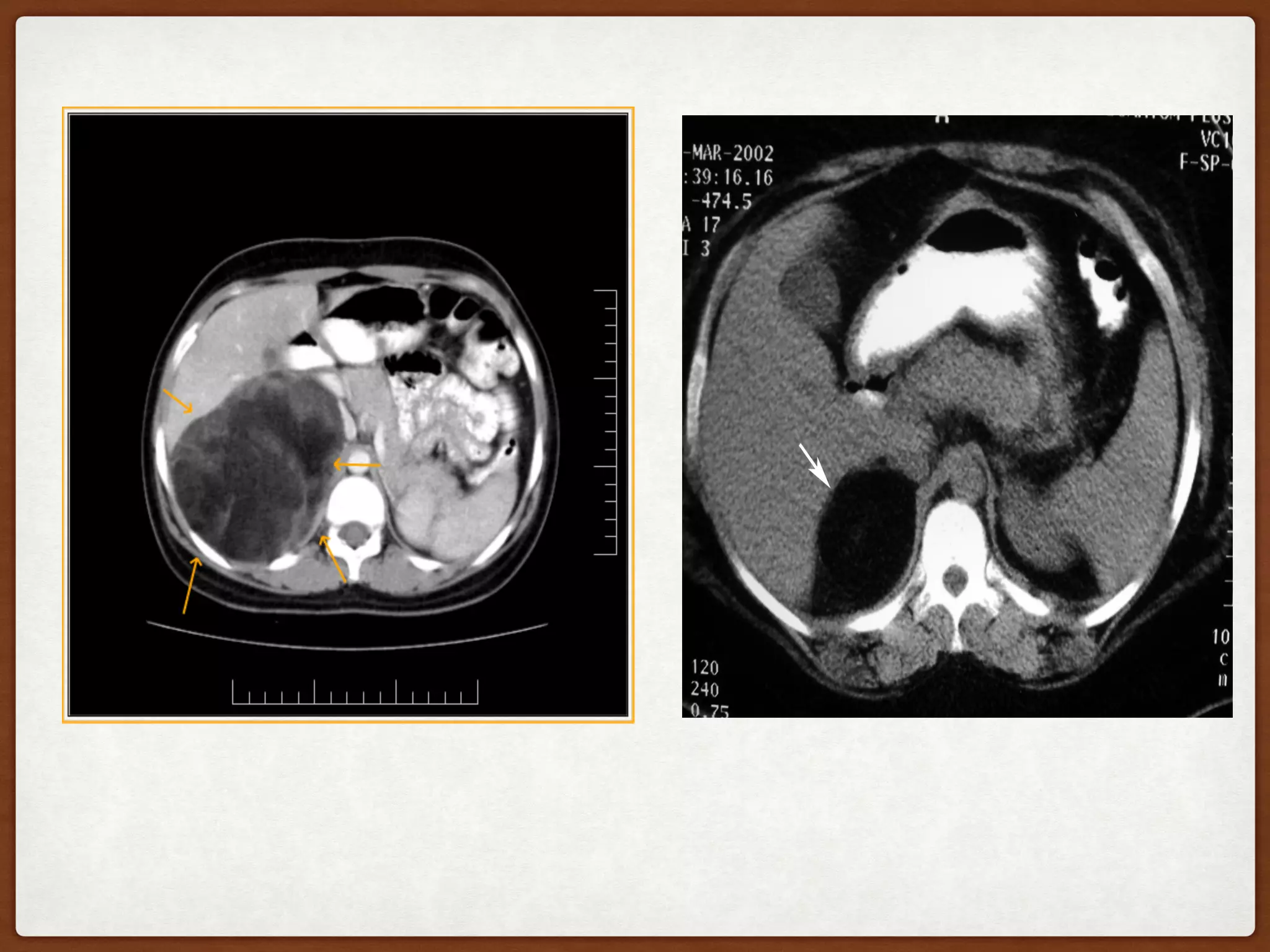
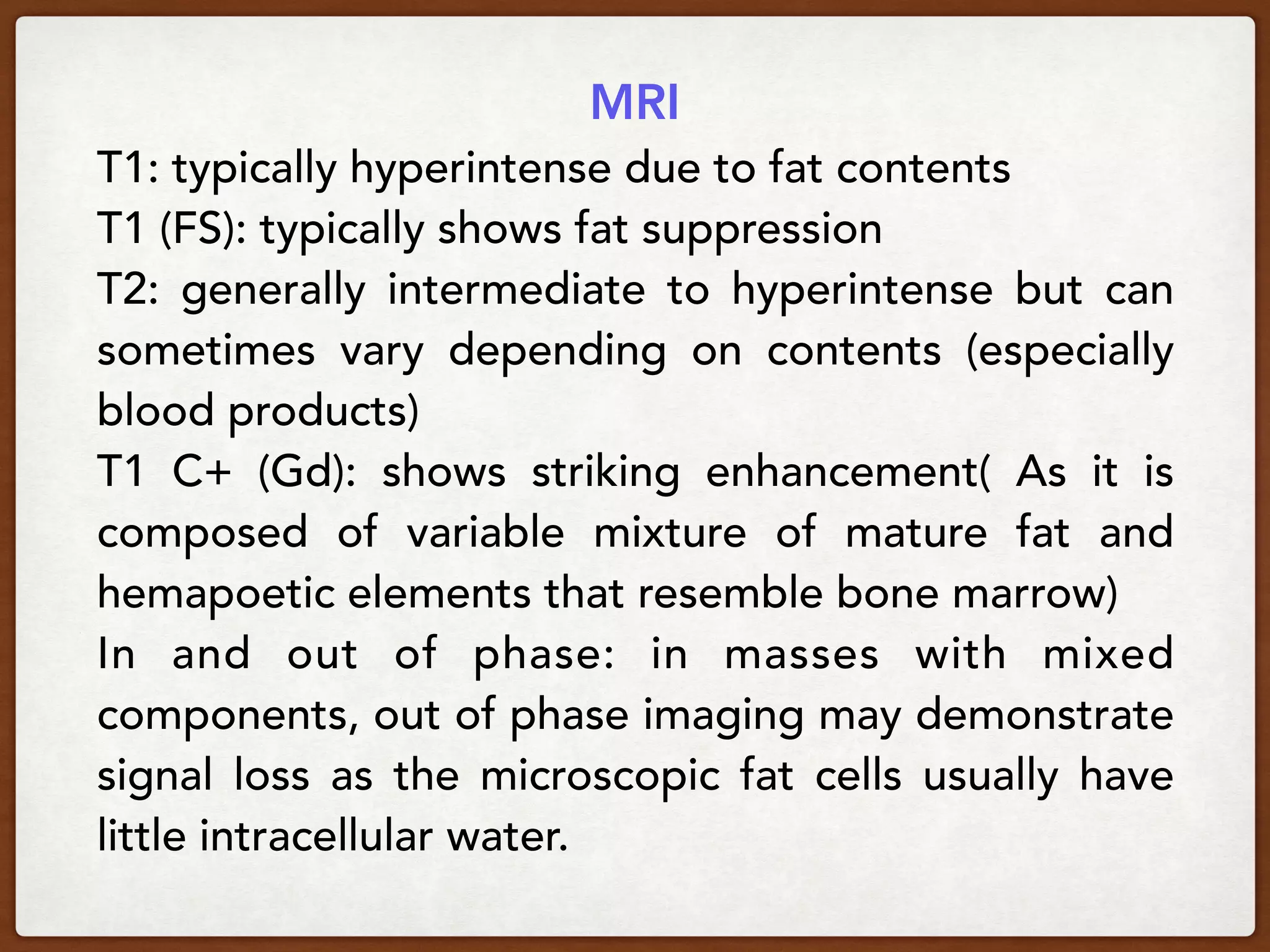
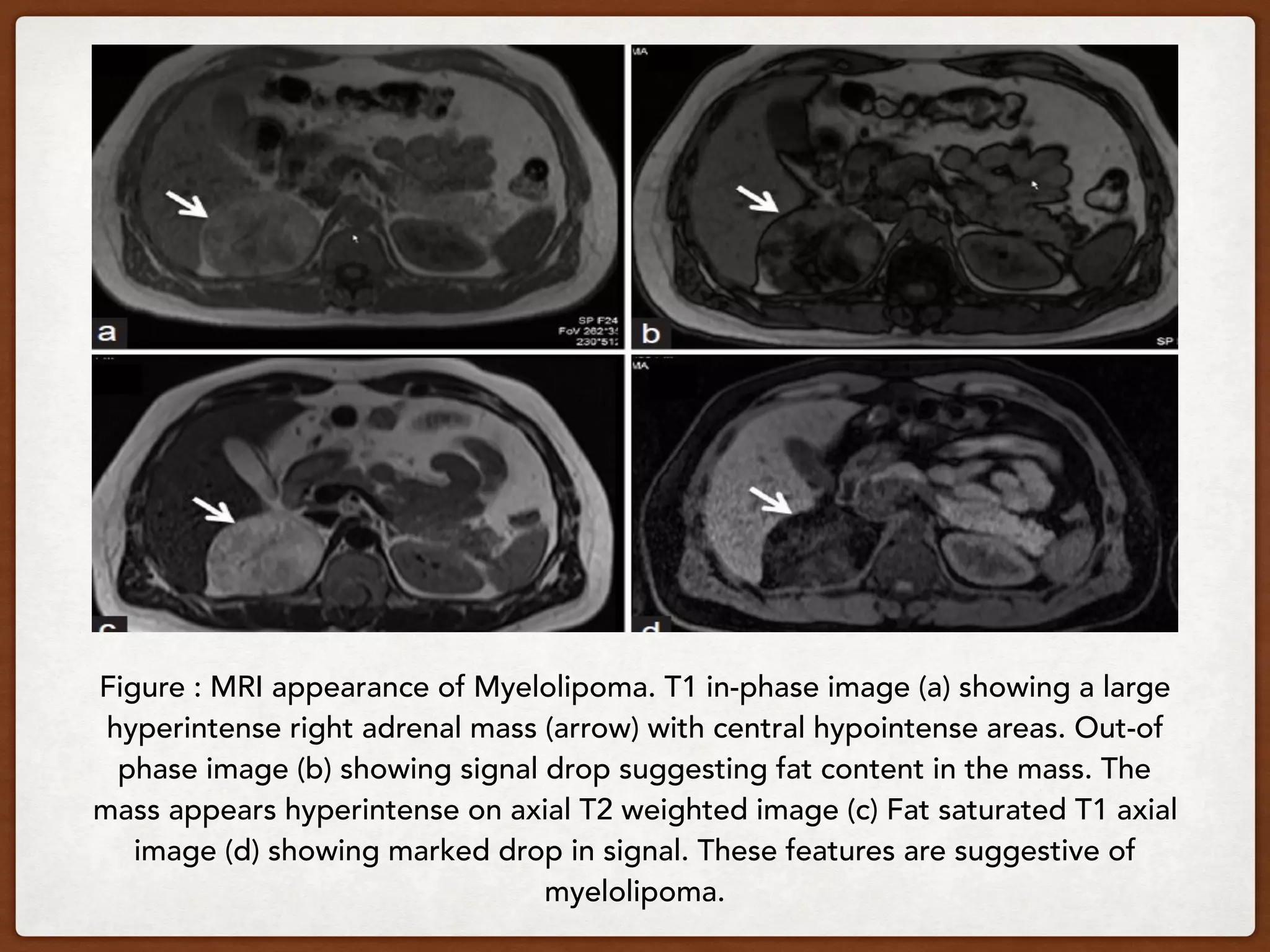
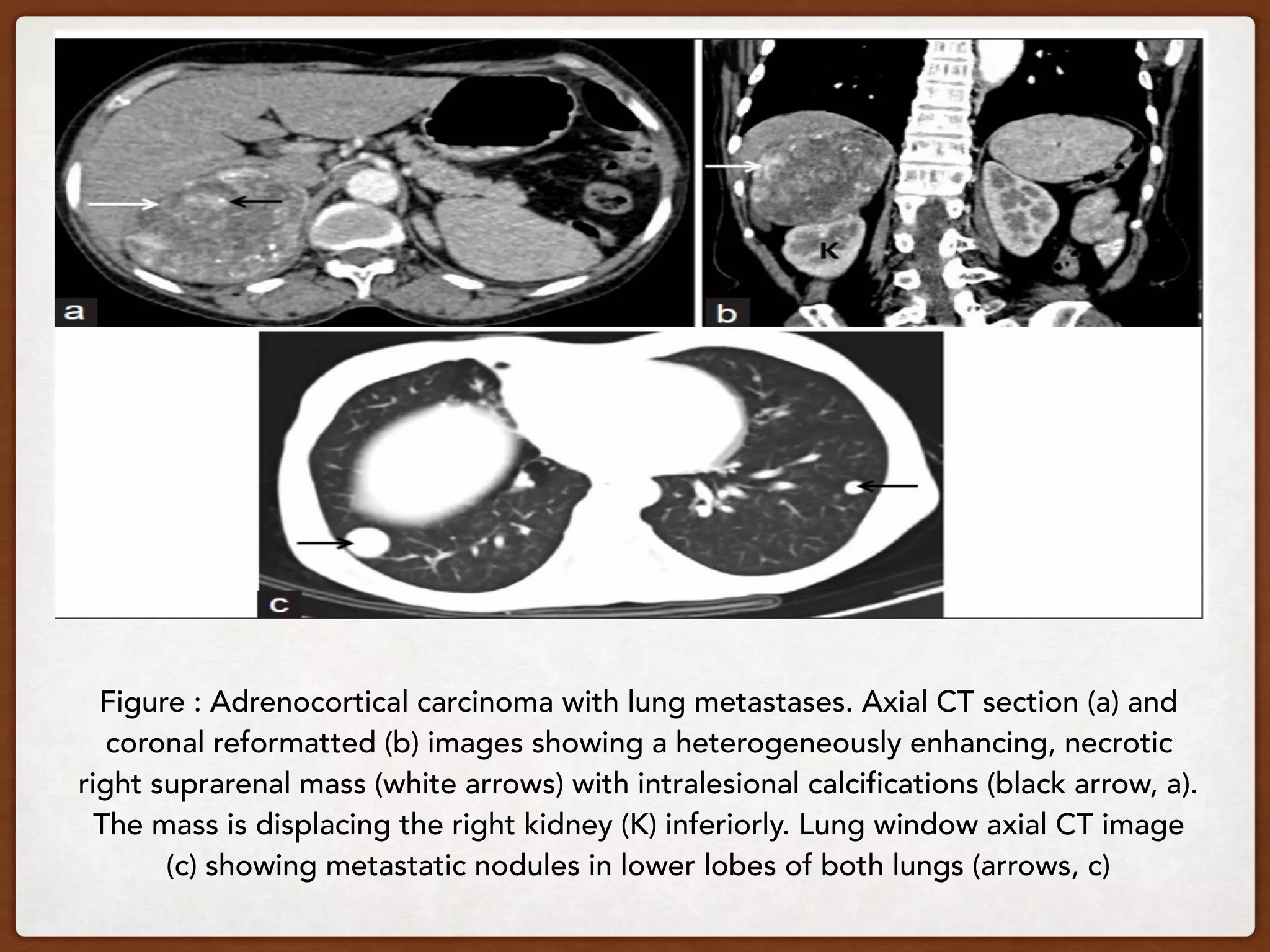
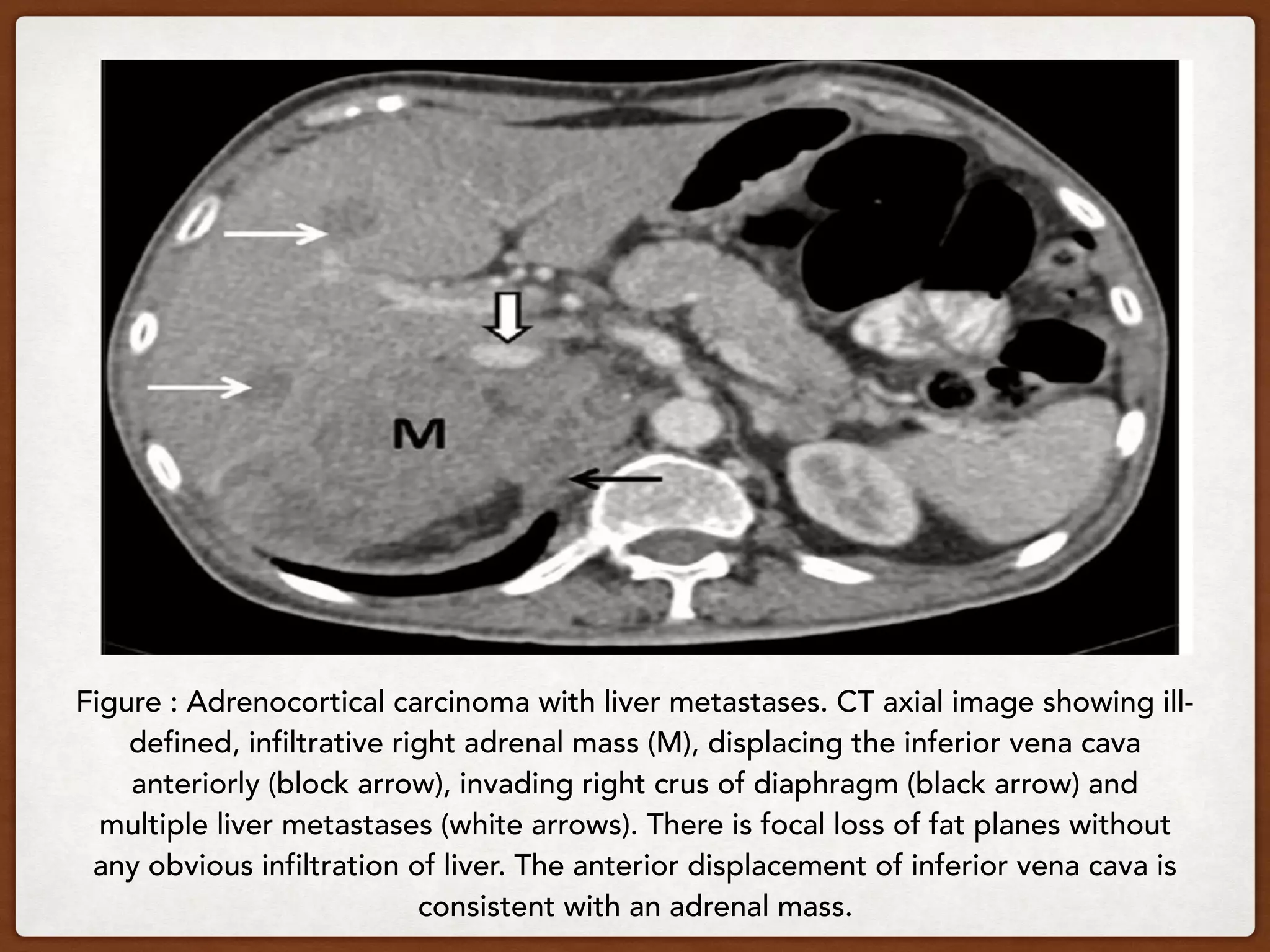
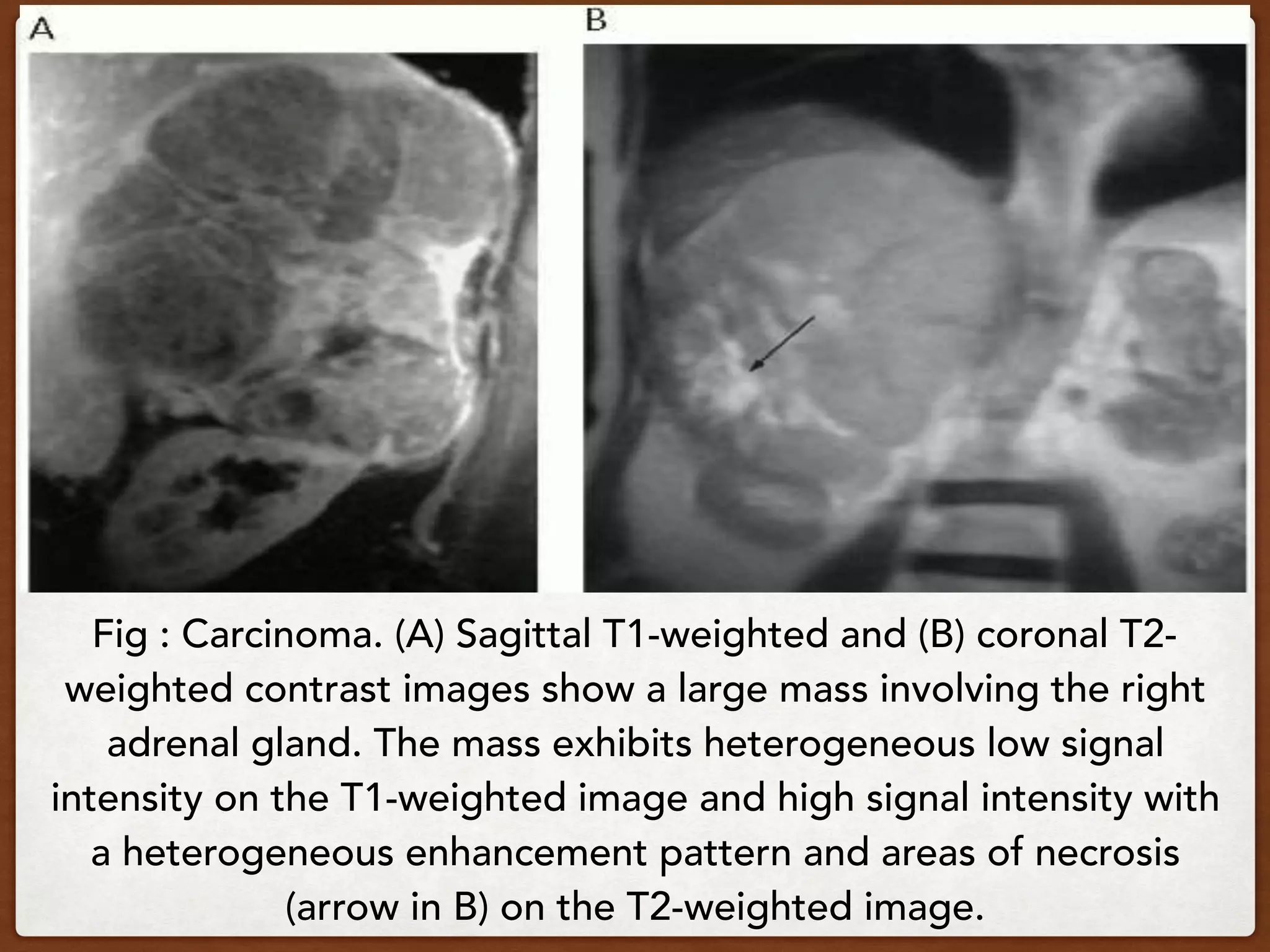
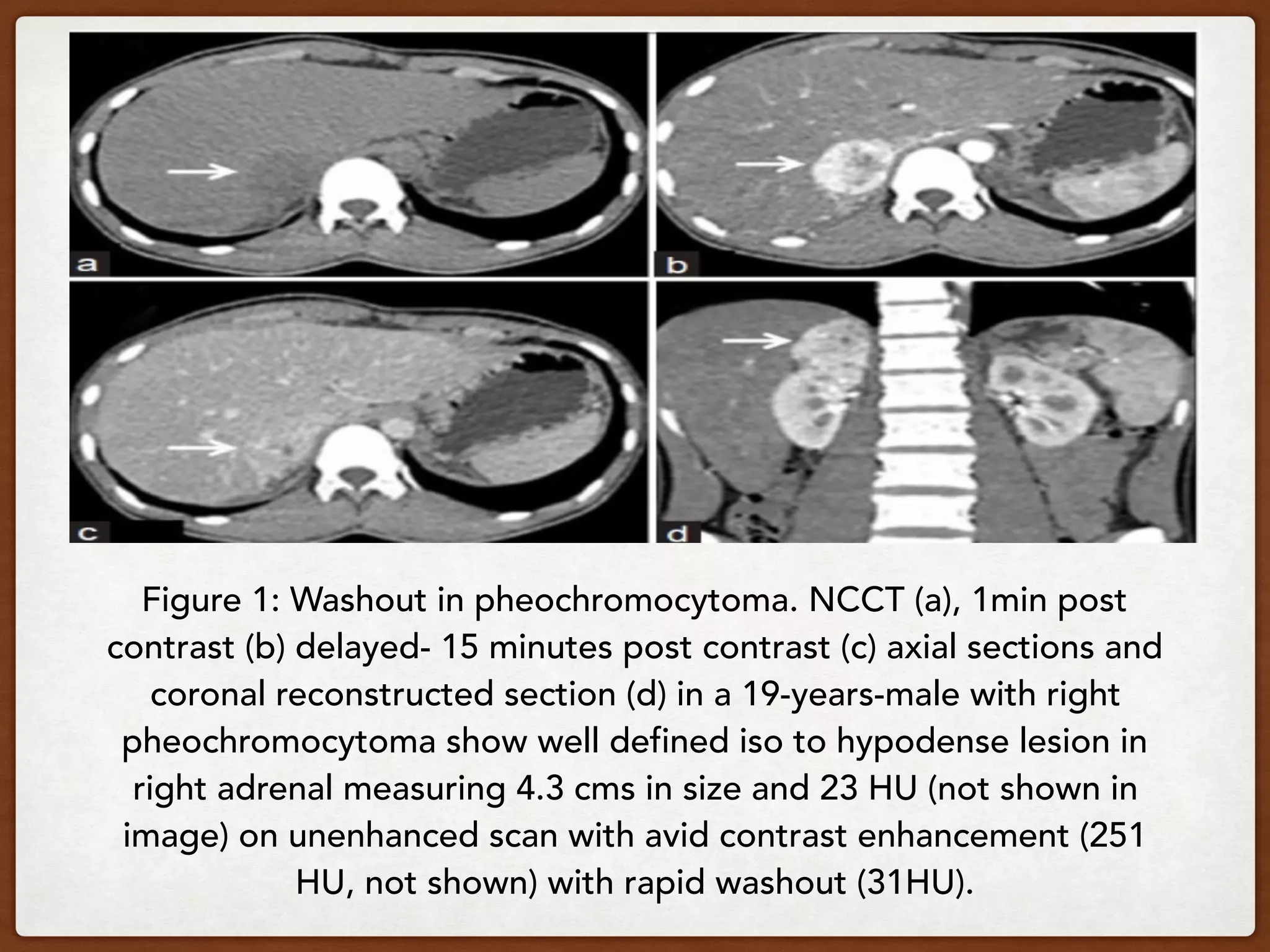
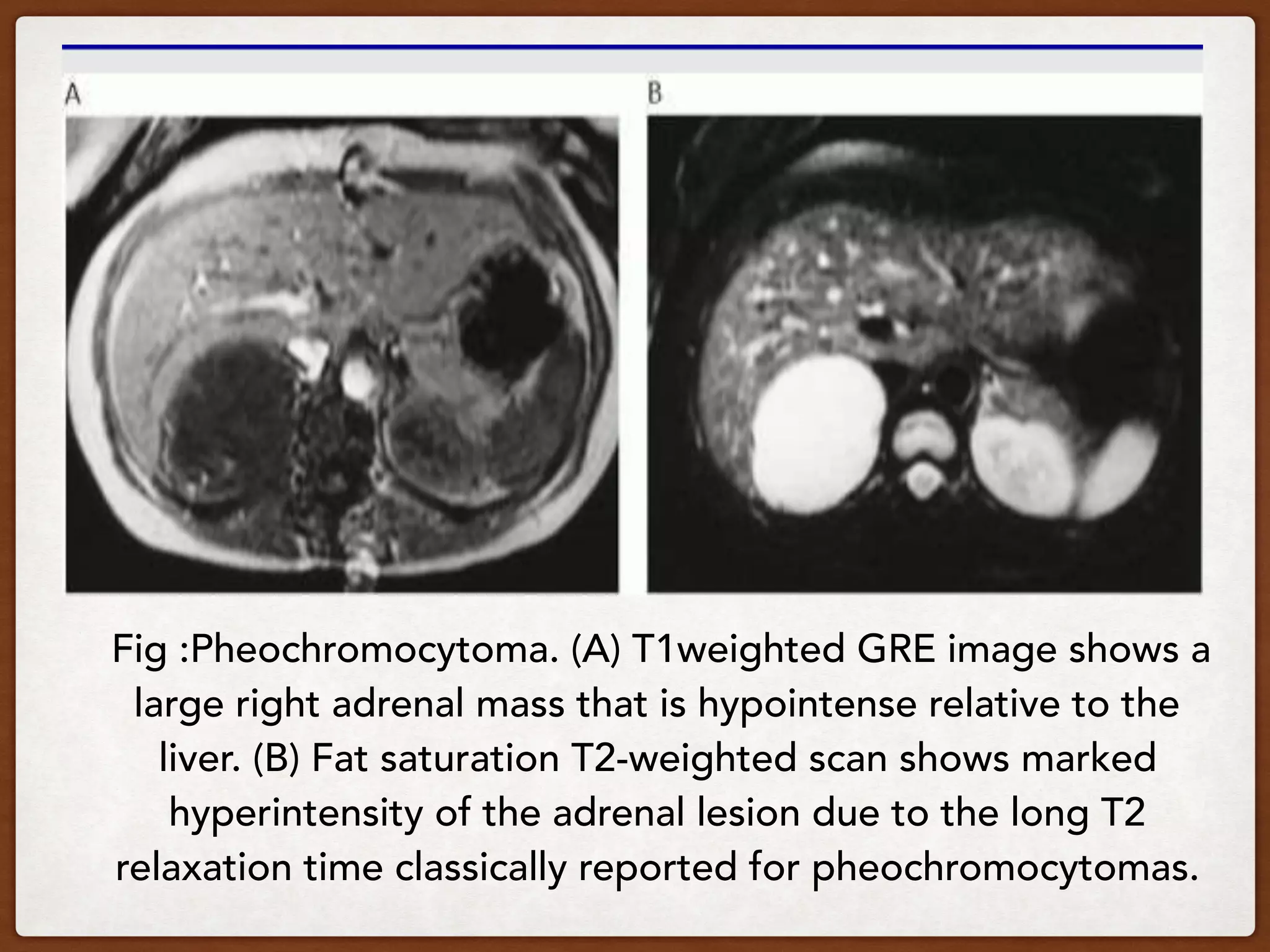
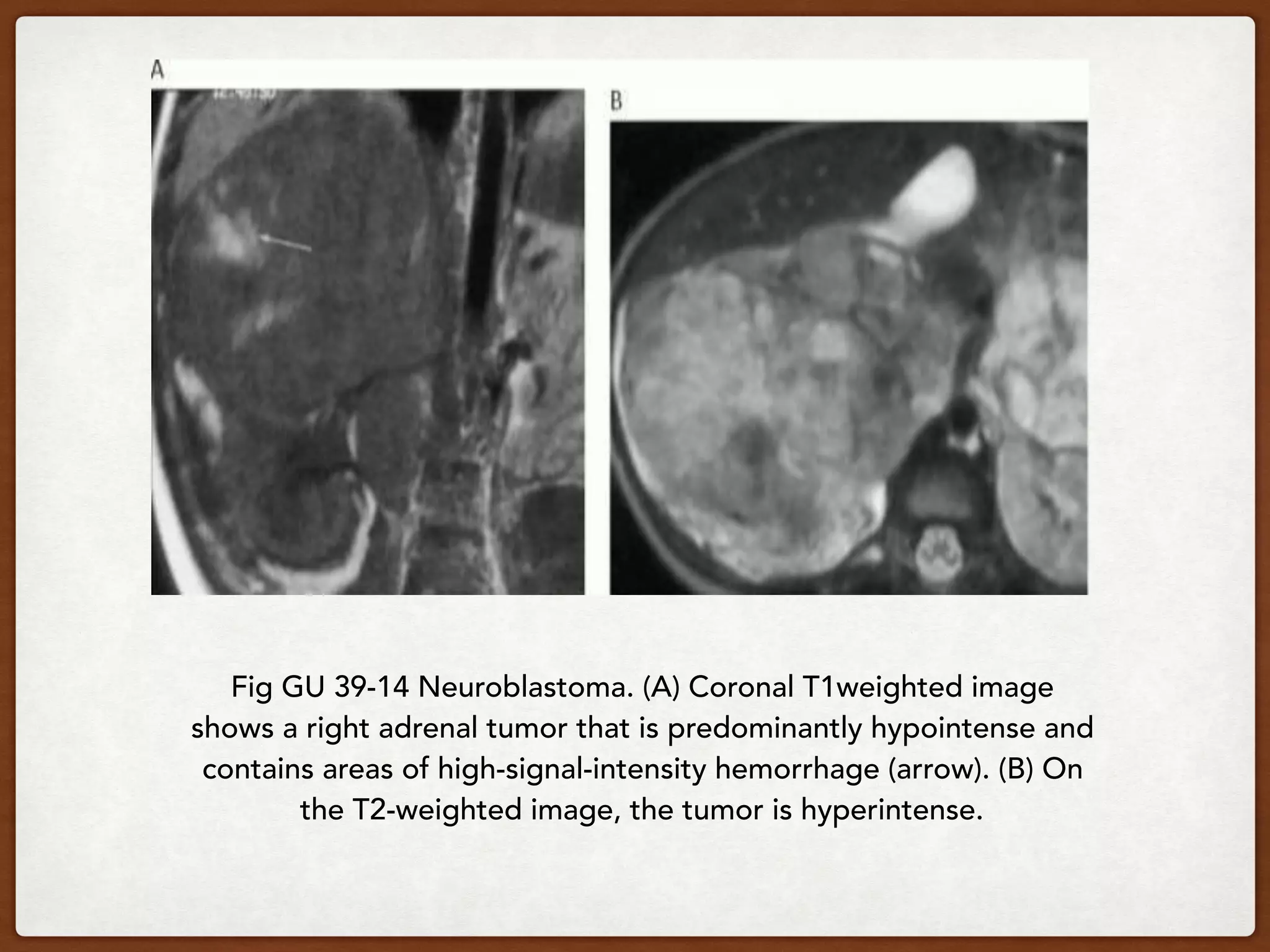
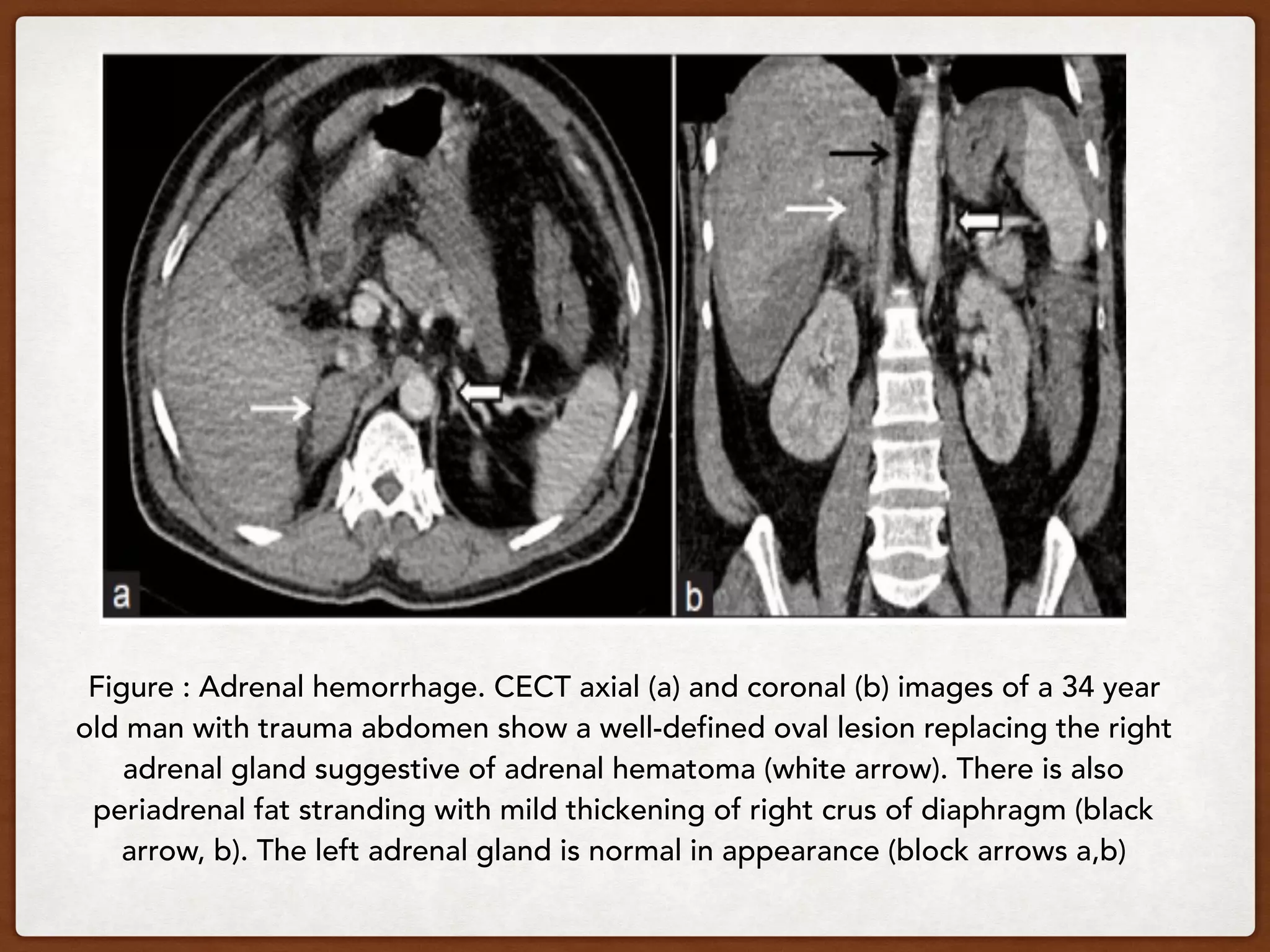
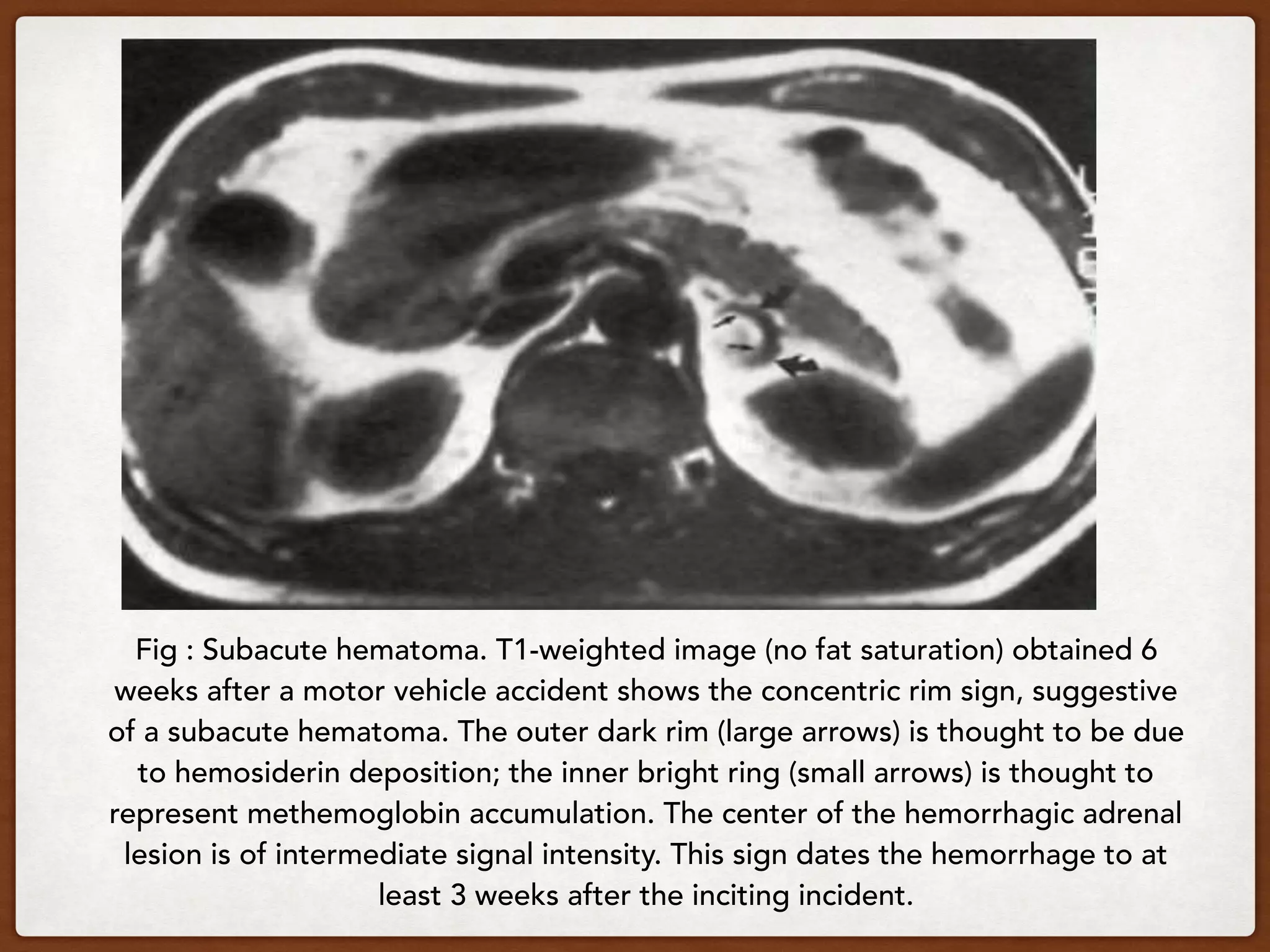
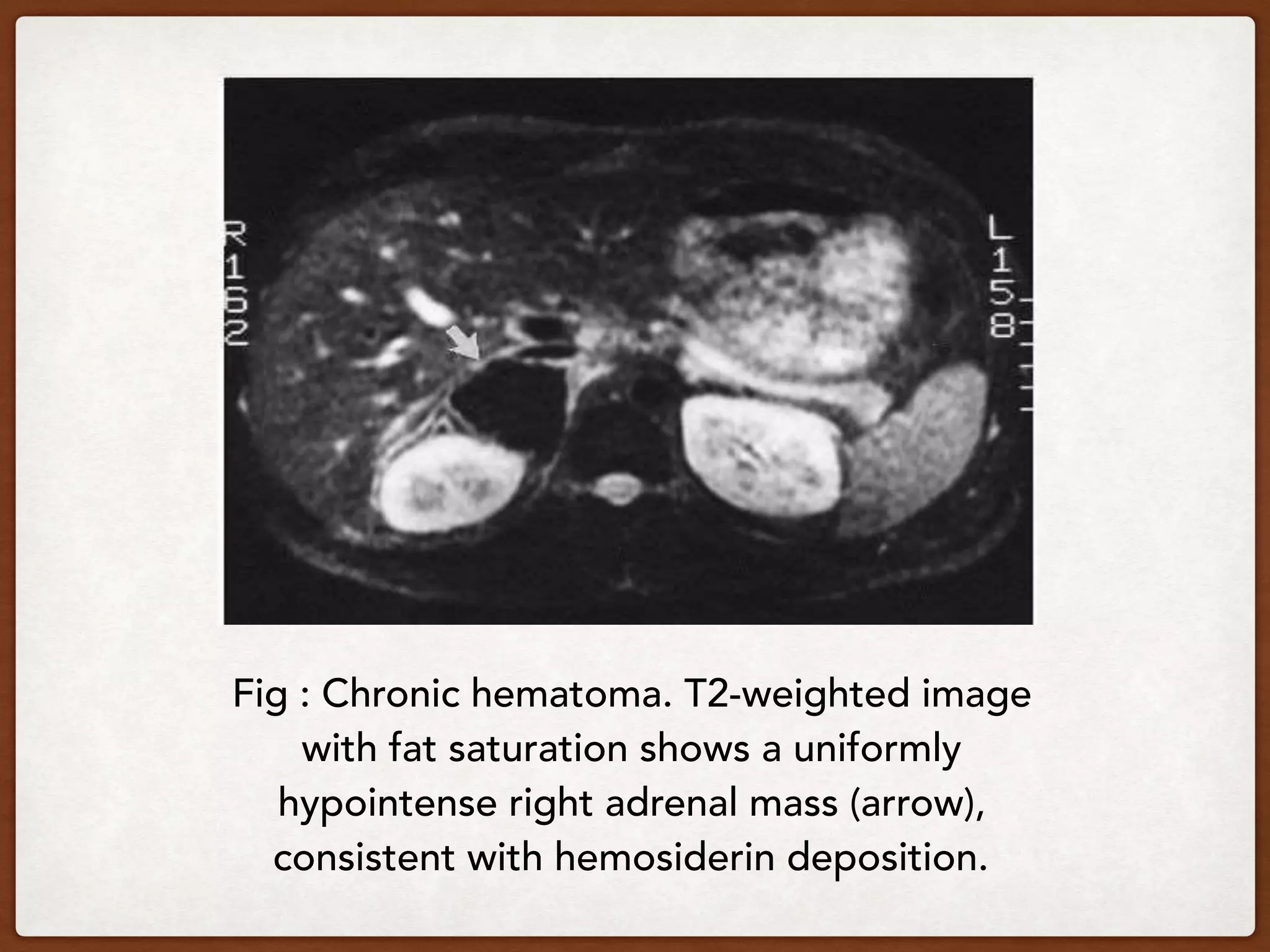
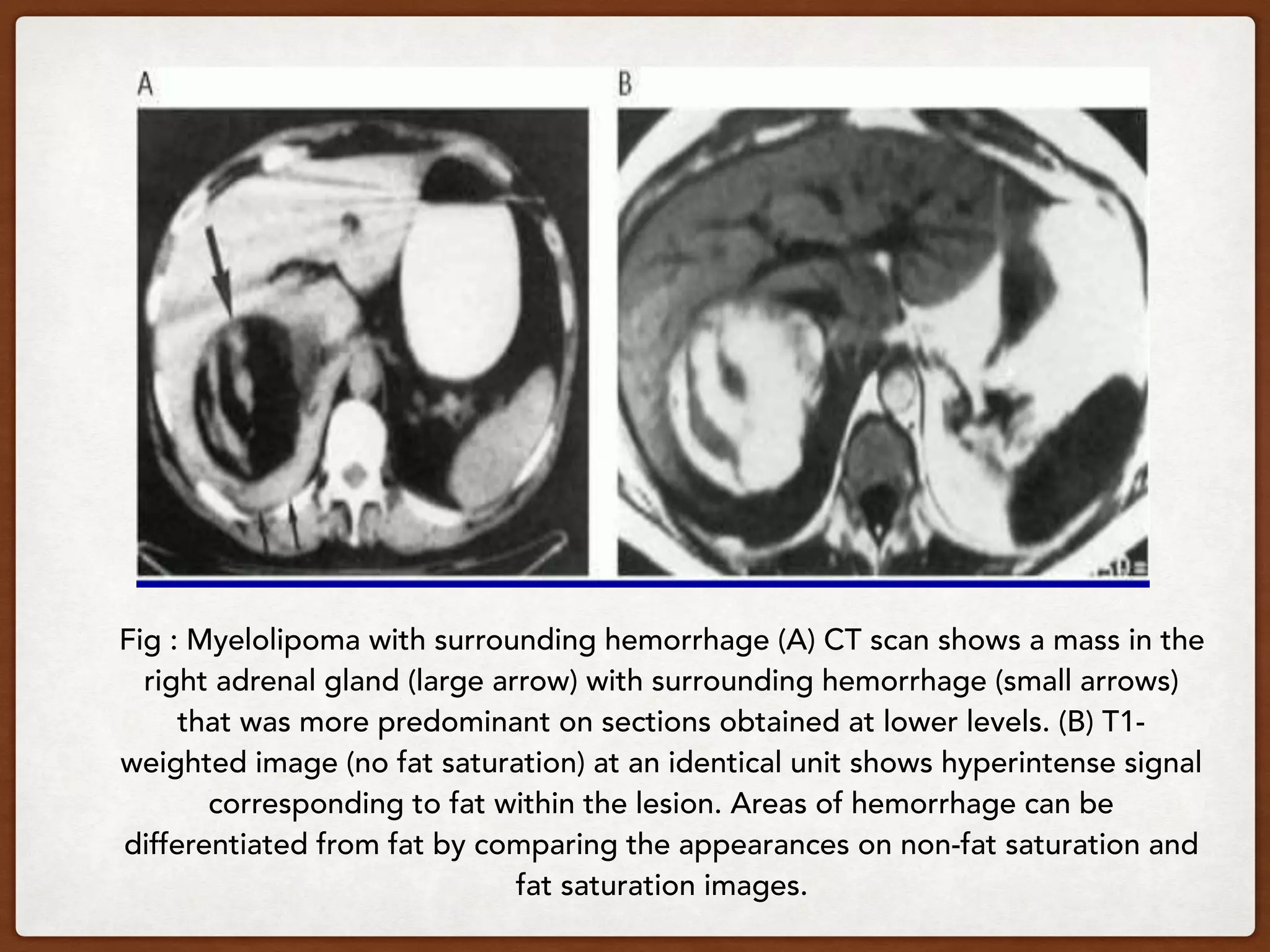
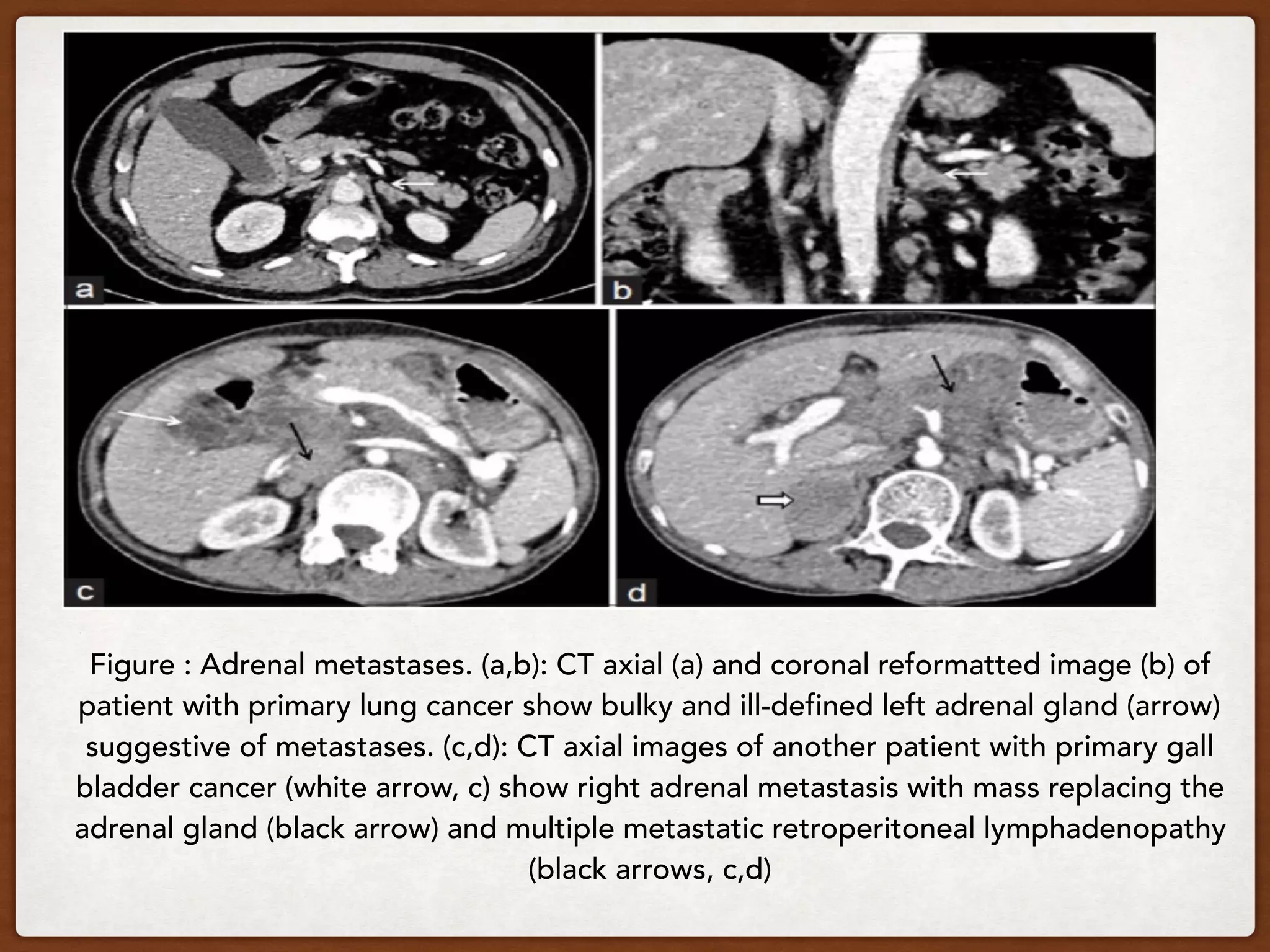
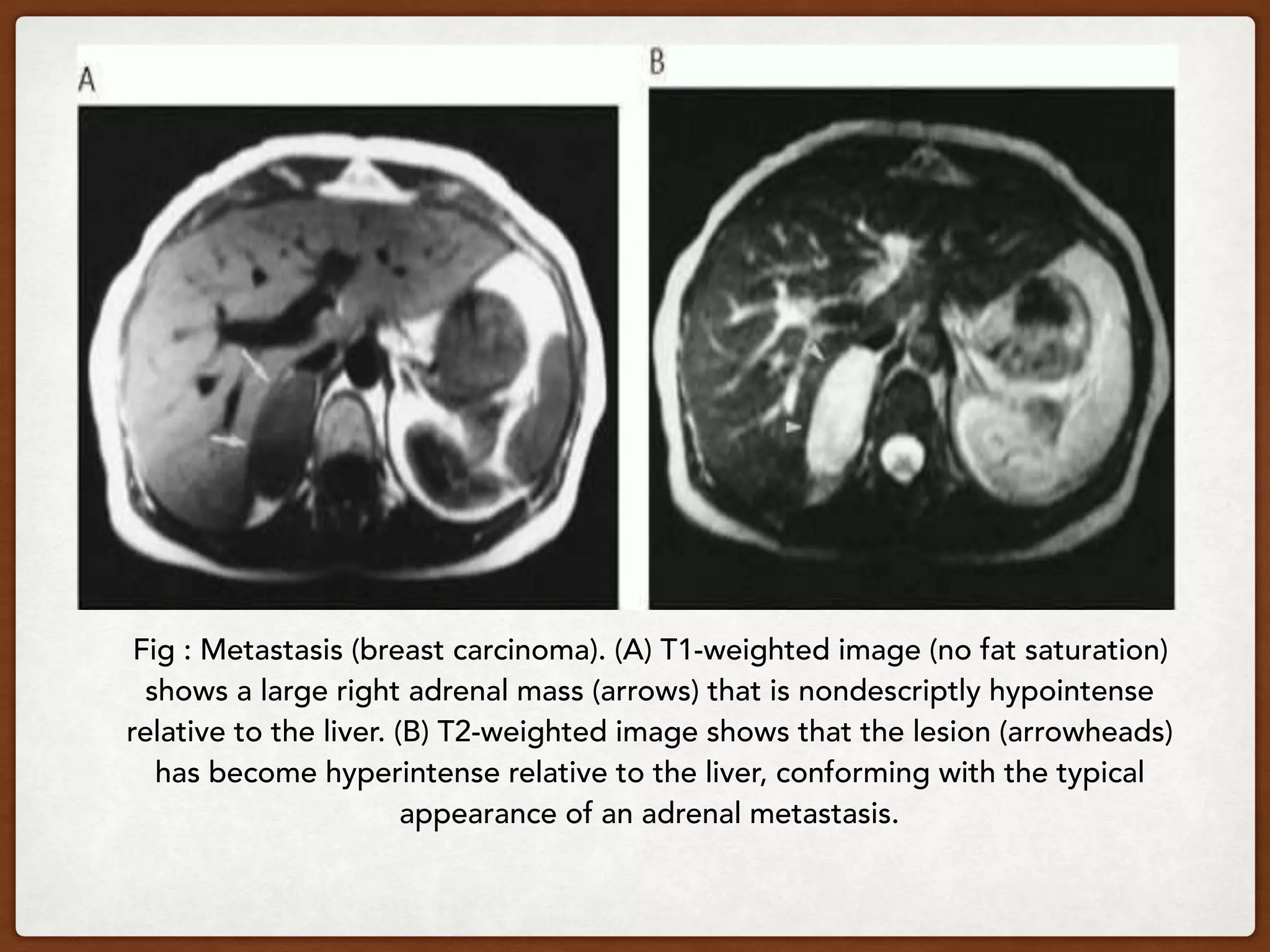
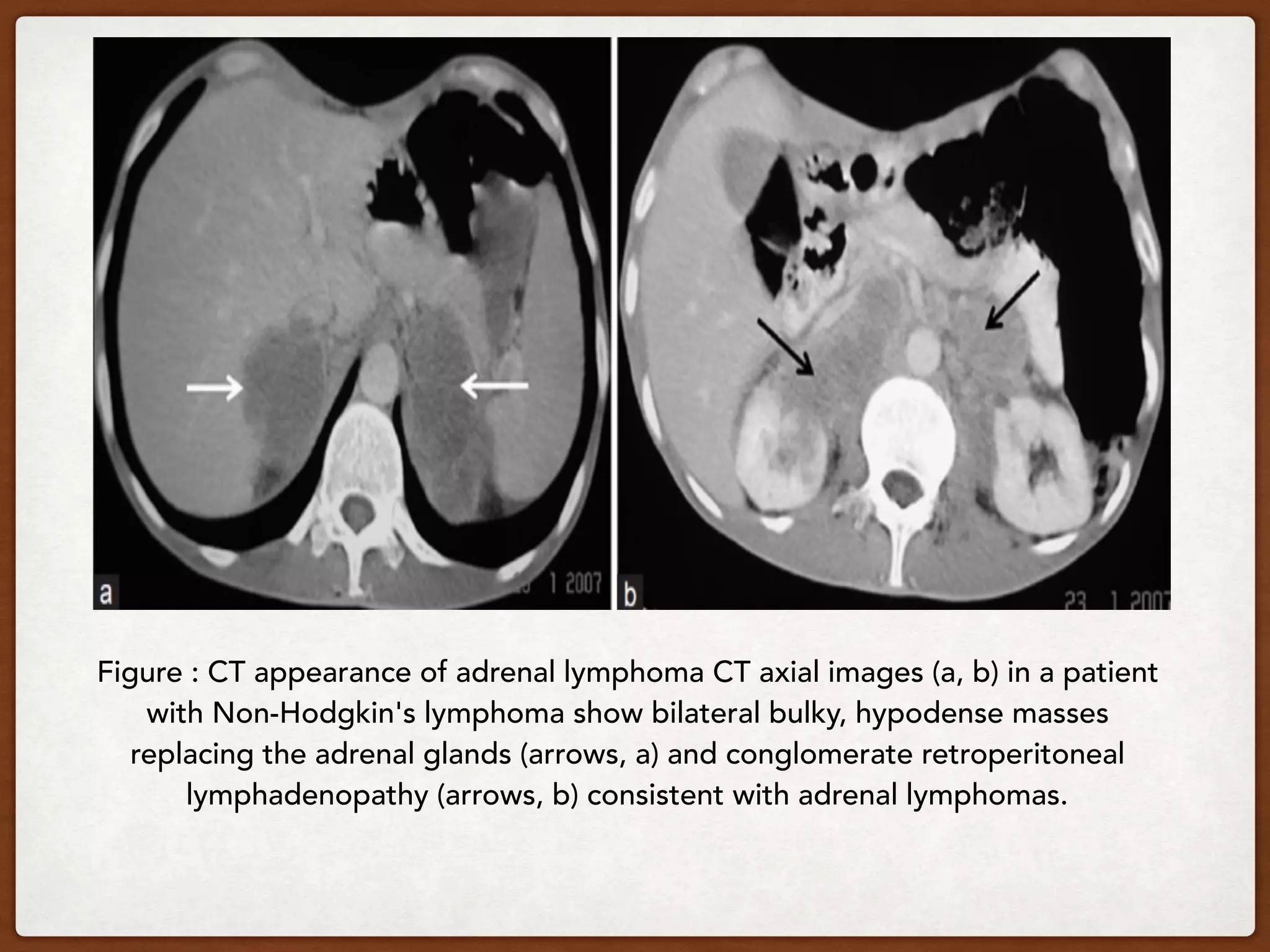
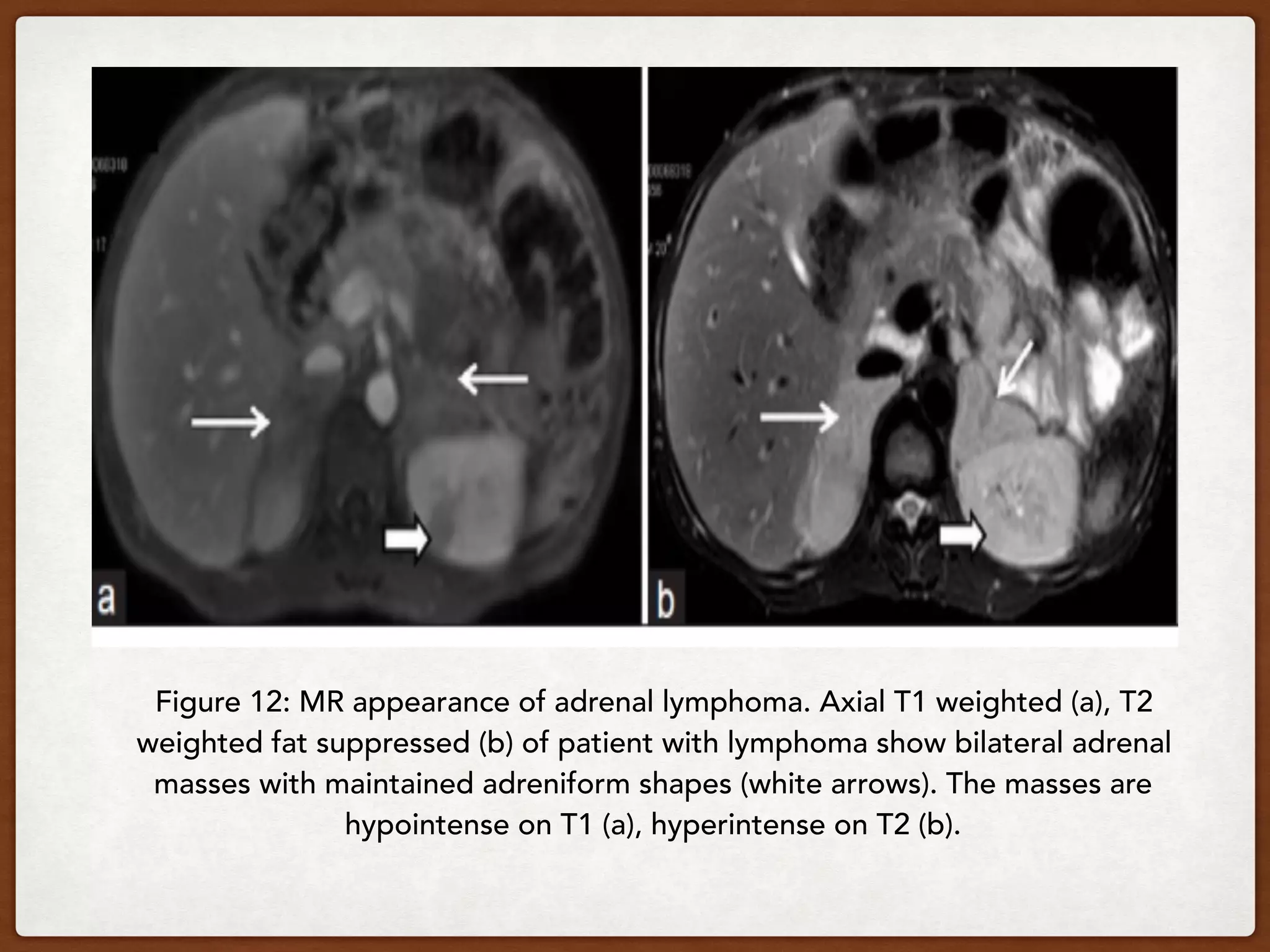
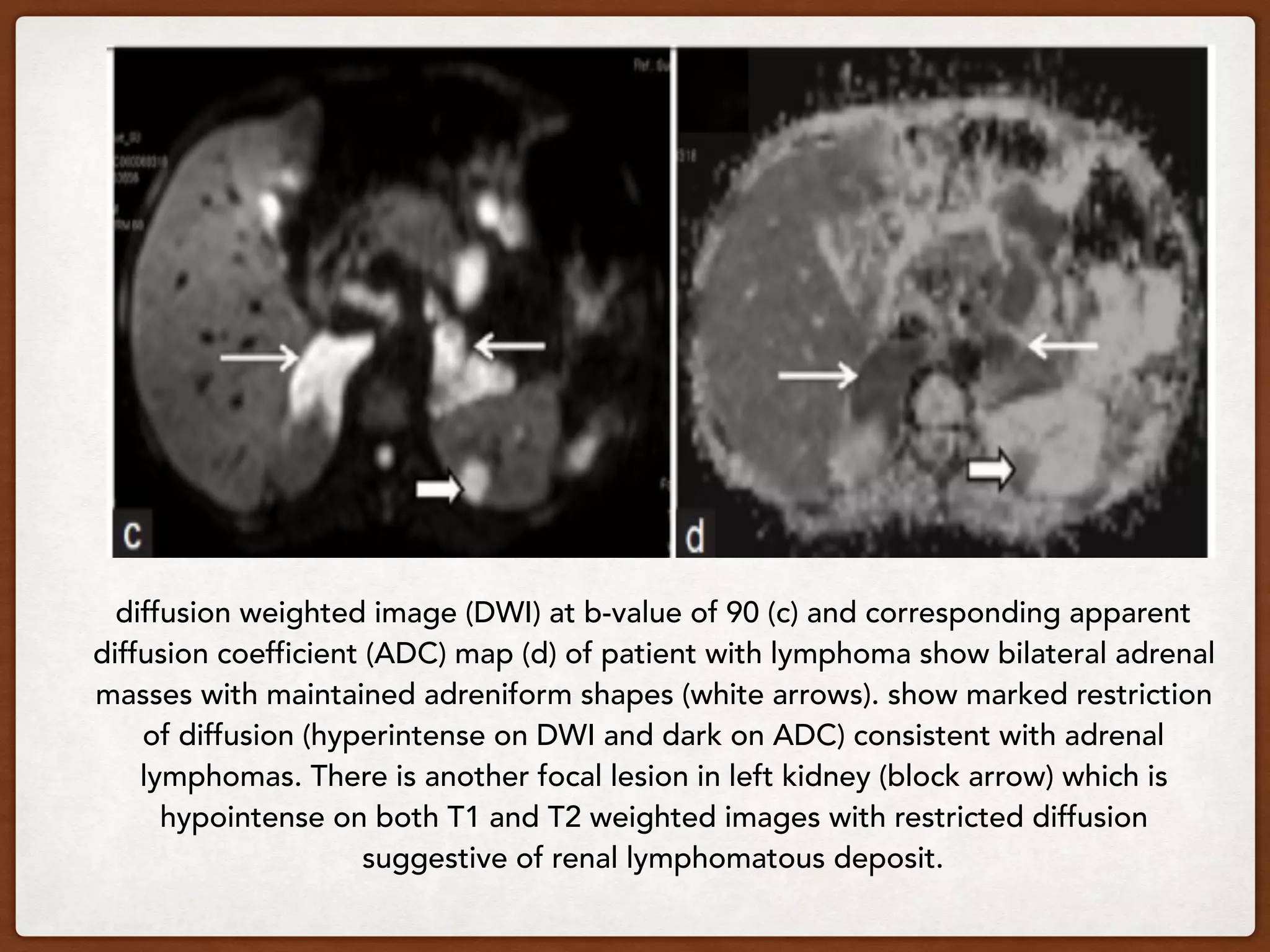
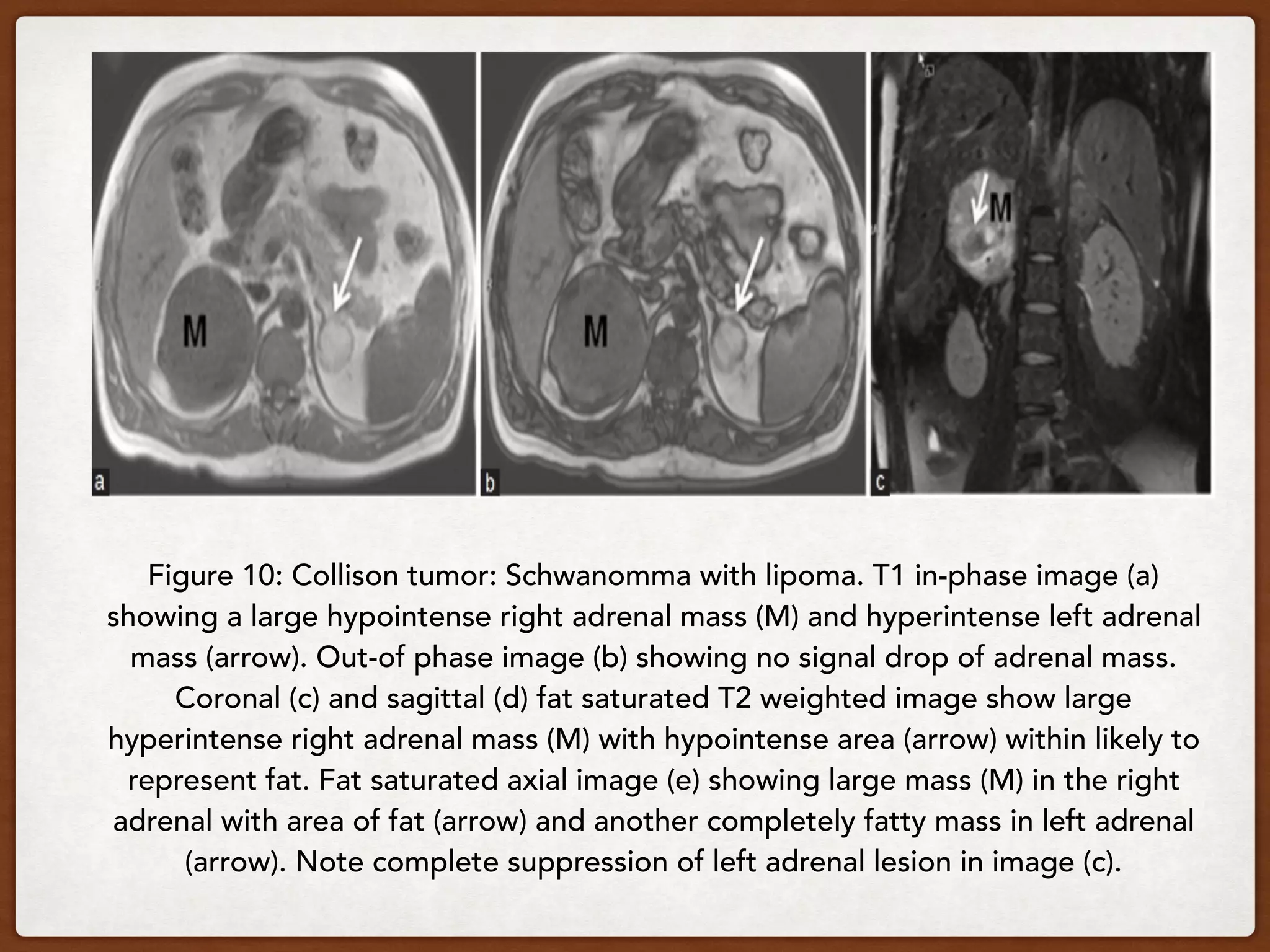
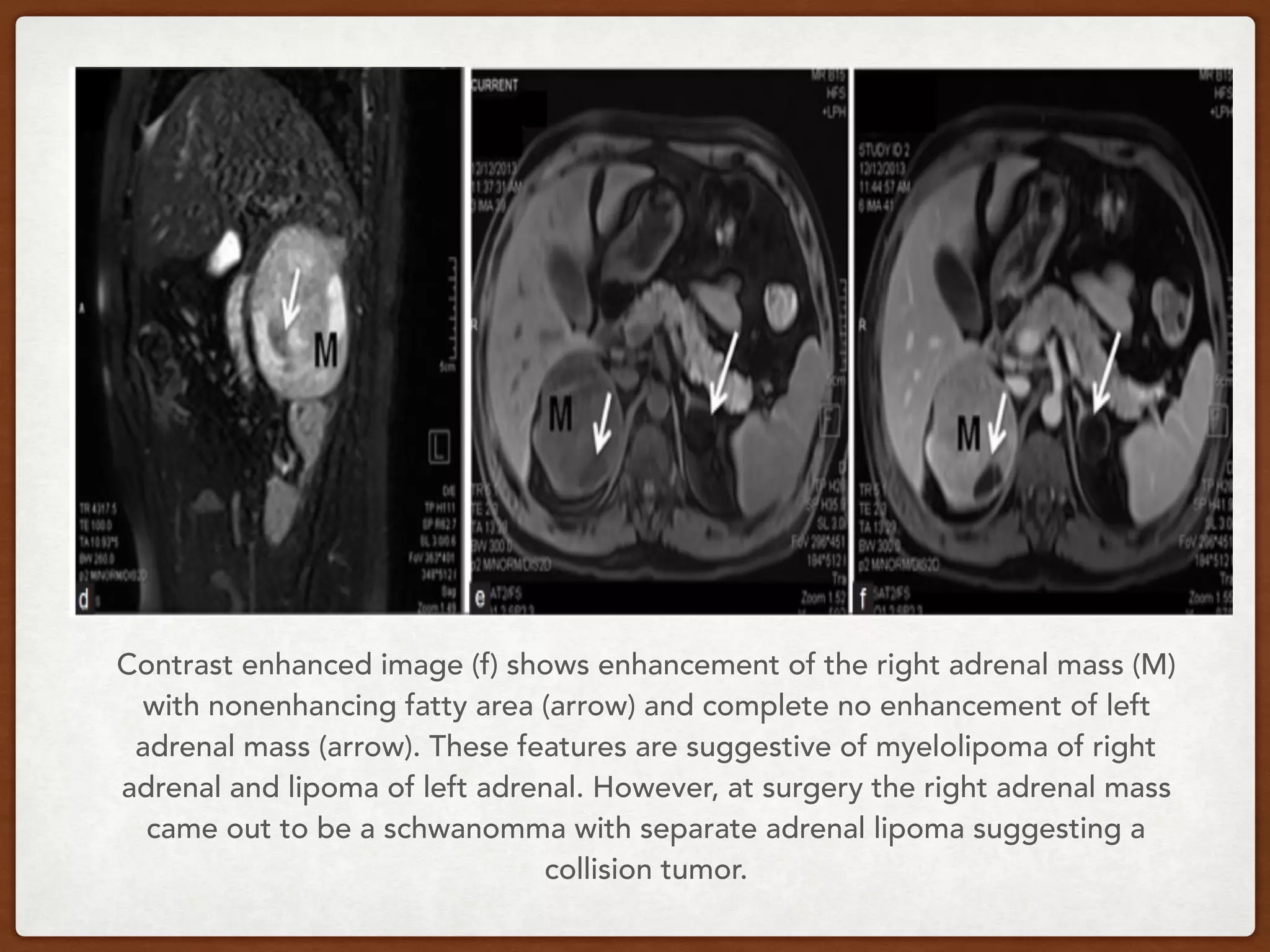
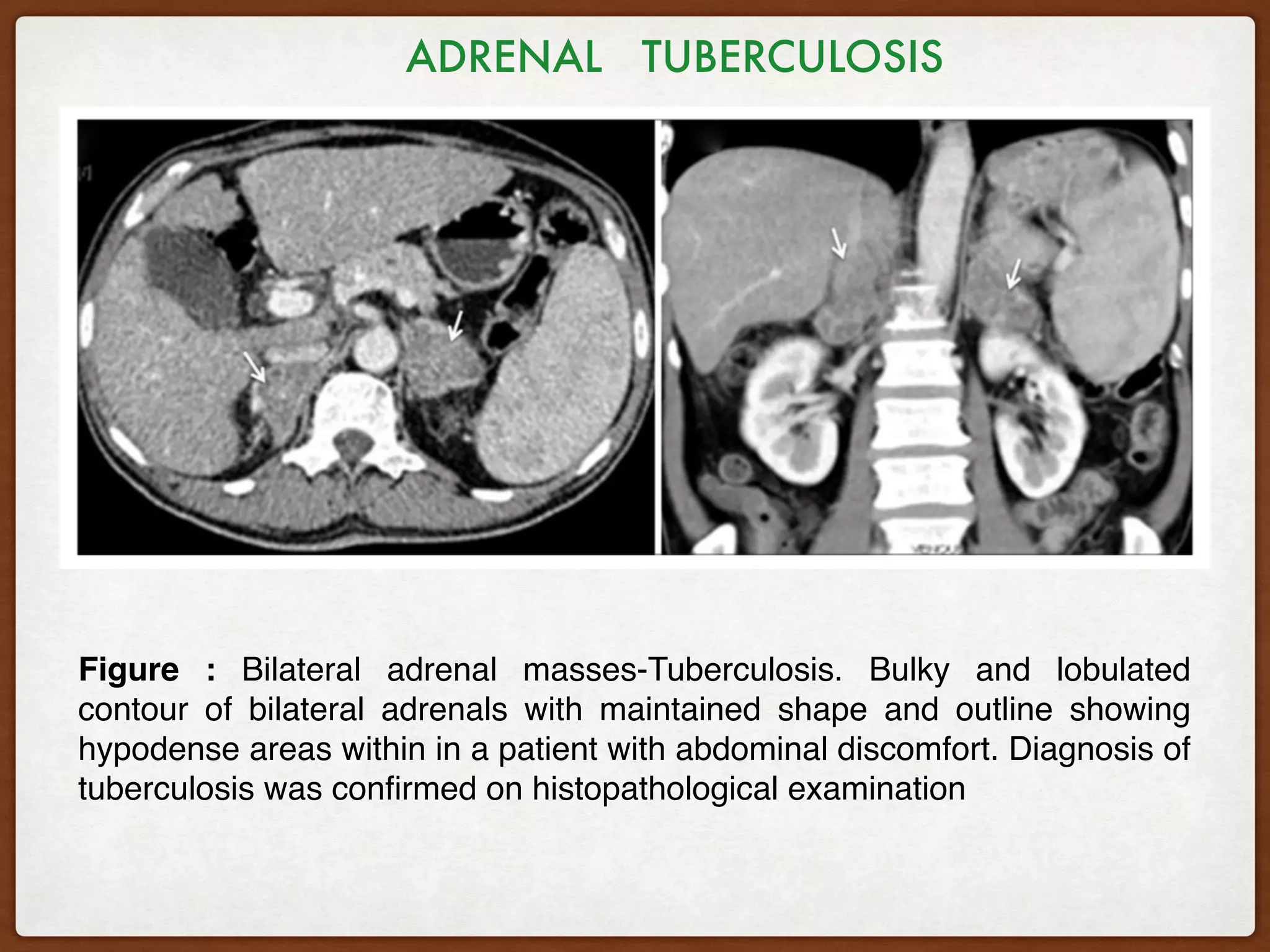
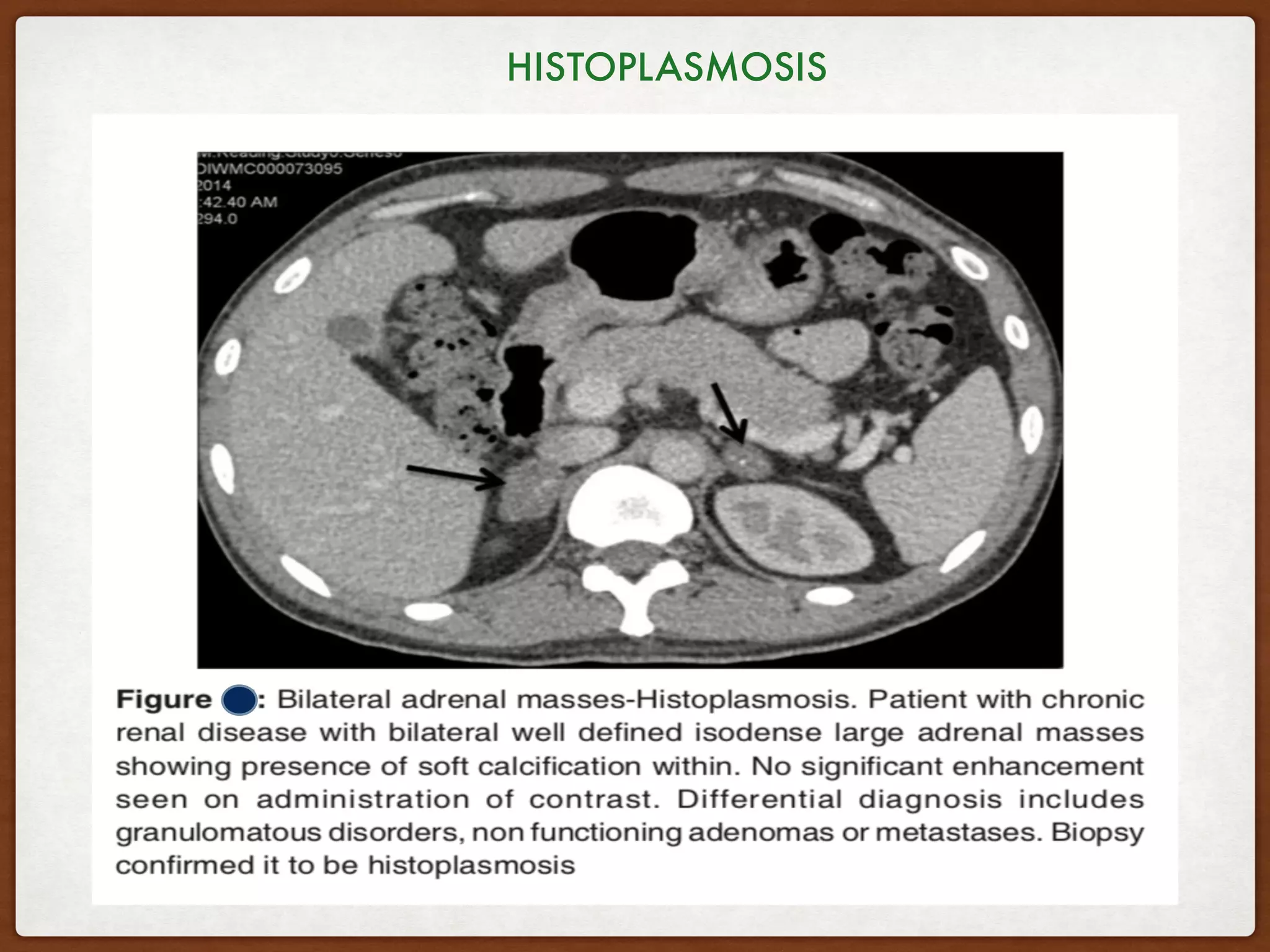
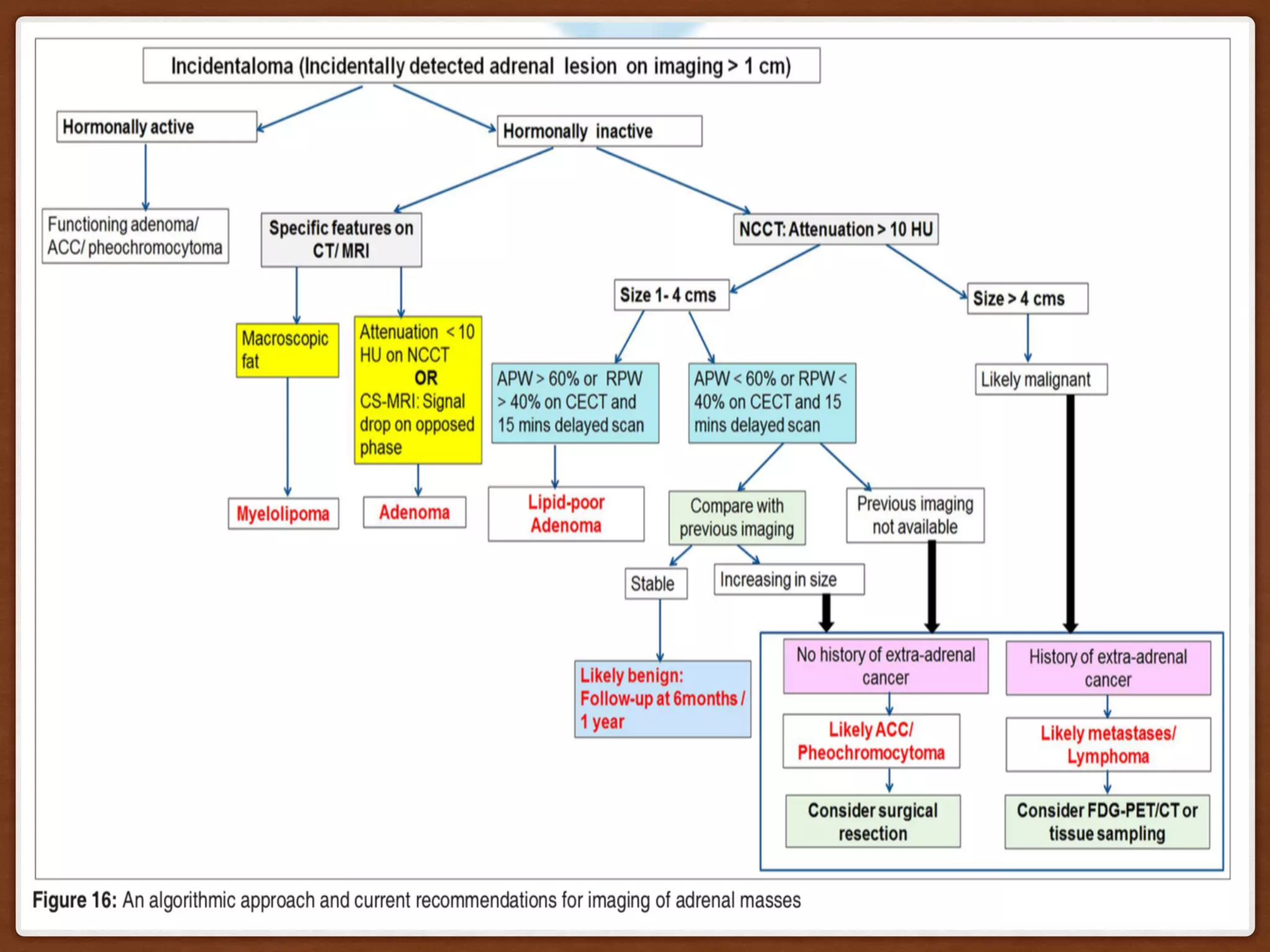
The document discusses various types of adrenal masses and how they appear on different imaging modalities like CT, MRI, and ultrasound. It describes the normal anatomy of the adrenal glands and then discusses common benign and malignant adrenal masses. Some key masses mentioned include adrenal adenomas, pheochromocytomas, adrenocortical carcinomas, myelolipomas, and neuroblastomas. Imaging features discussed help differentiate between these different adrenal lesions.