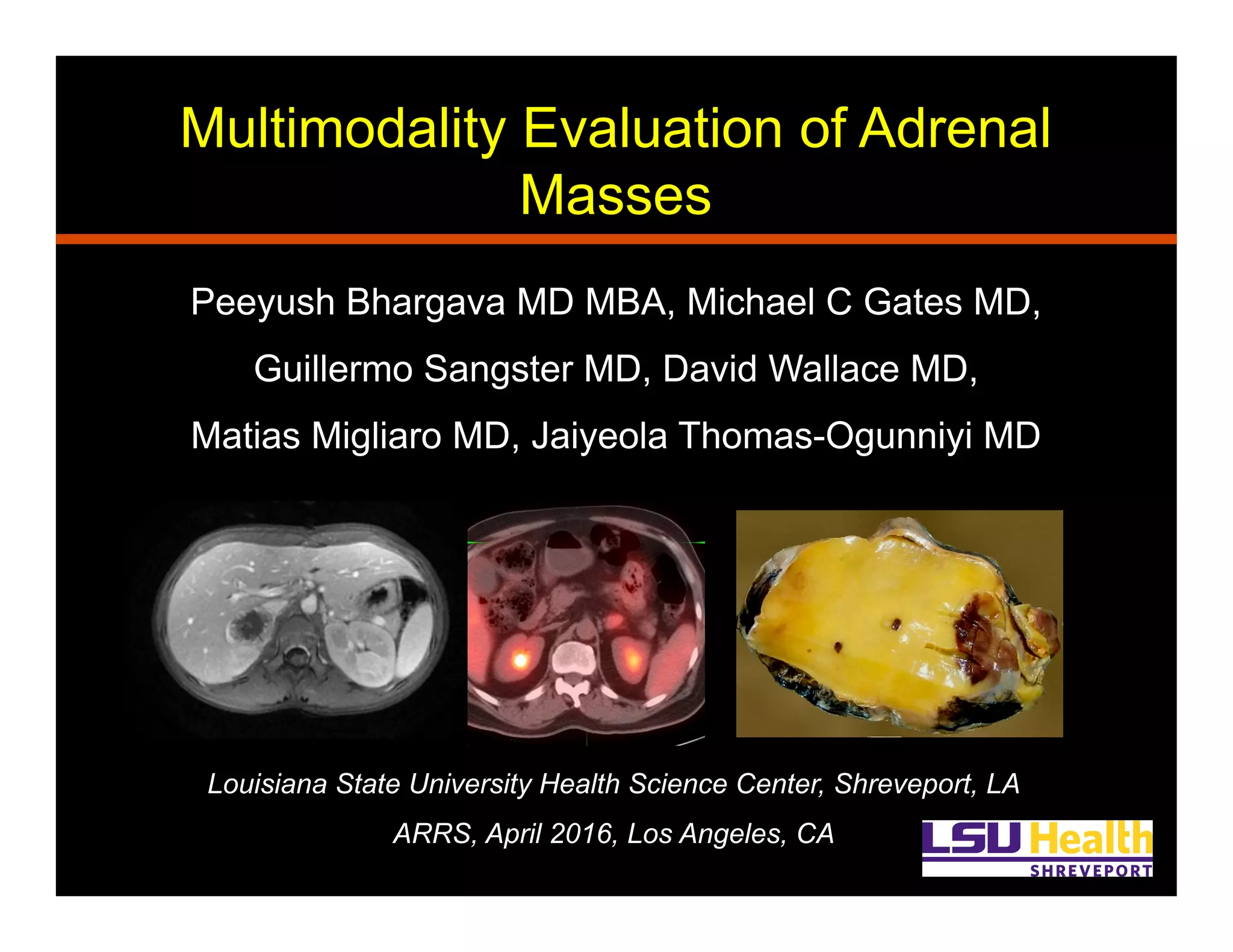
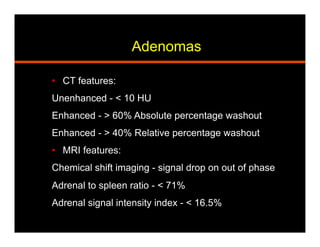
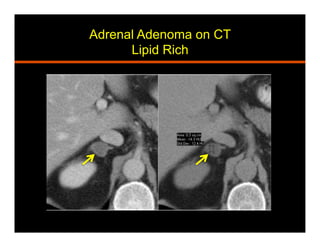
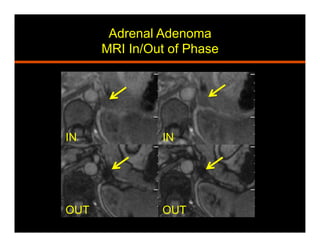
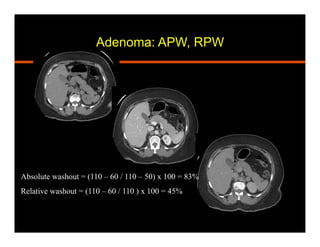
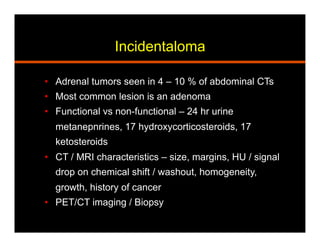
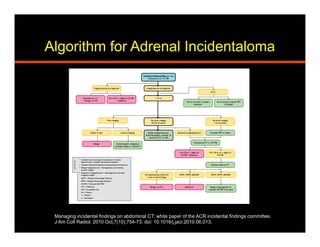
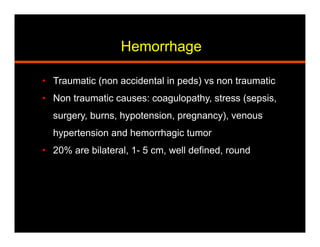
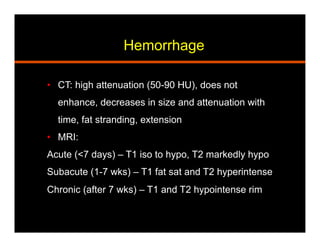
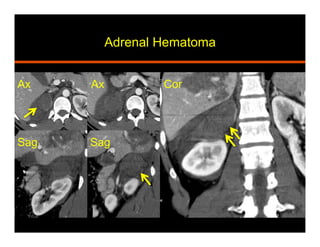
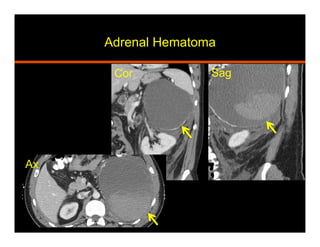
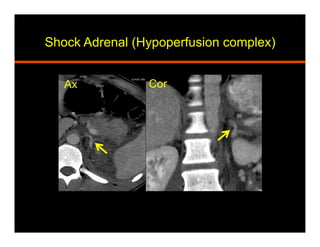
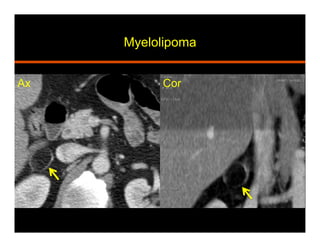
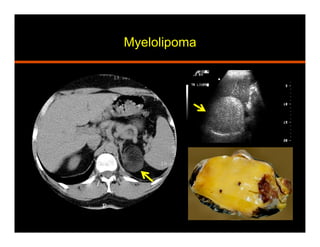
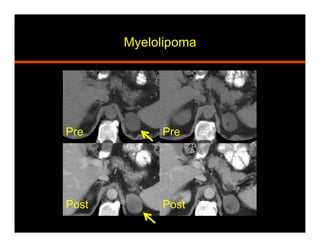
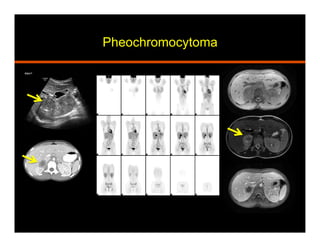
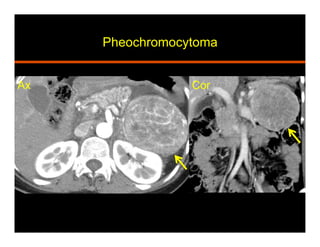
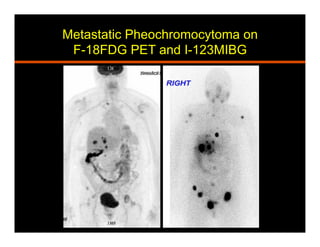
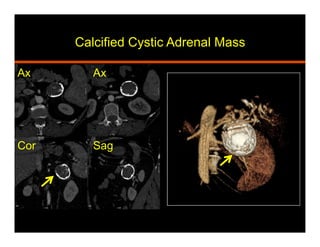
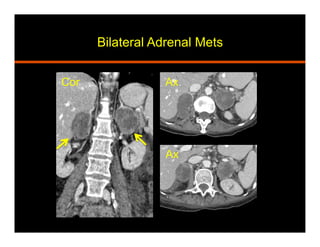
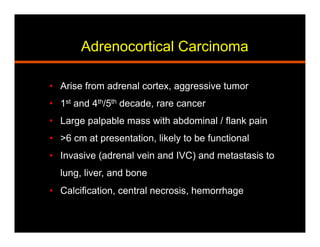
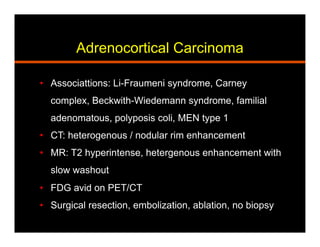
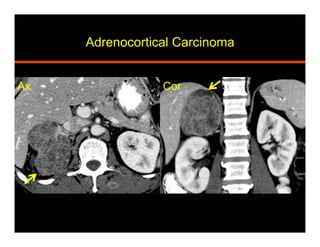
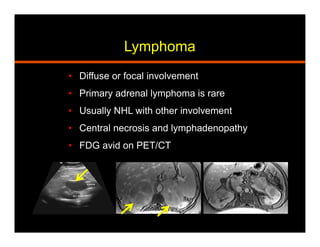
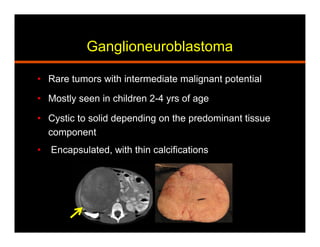
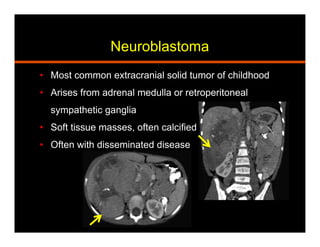
The document summarizes the multimodality evaluation of adrenal masses. It discusses the characteristic imaging findings of common benign and malignant adrenal masses using CT, MRI, PET, and other imaging modalities. The goals are to review the spectrum of imaging findings and differentiate between benign and malignant adrenal masses. Common benign entities discussed include adenomas, hemorrhage, myelolipomas, pheochromocytomas, and cysts. Malignant entities covered are metastases, adrenocortical carcinomas, lymphomas, and others.