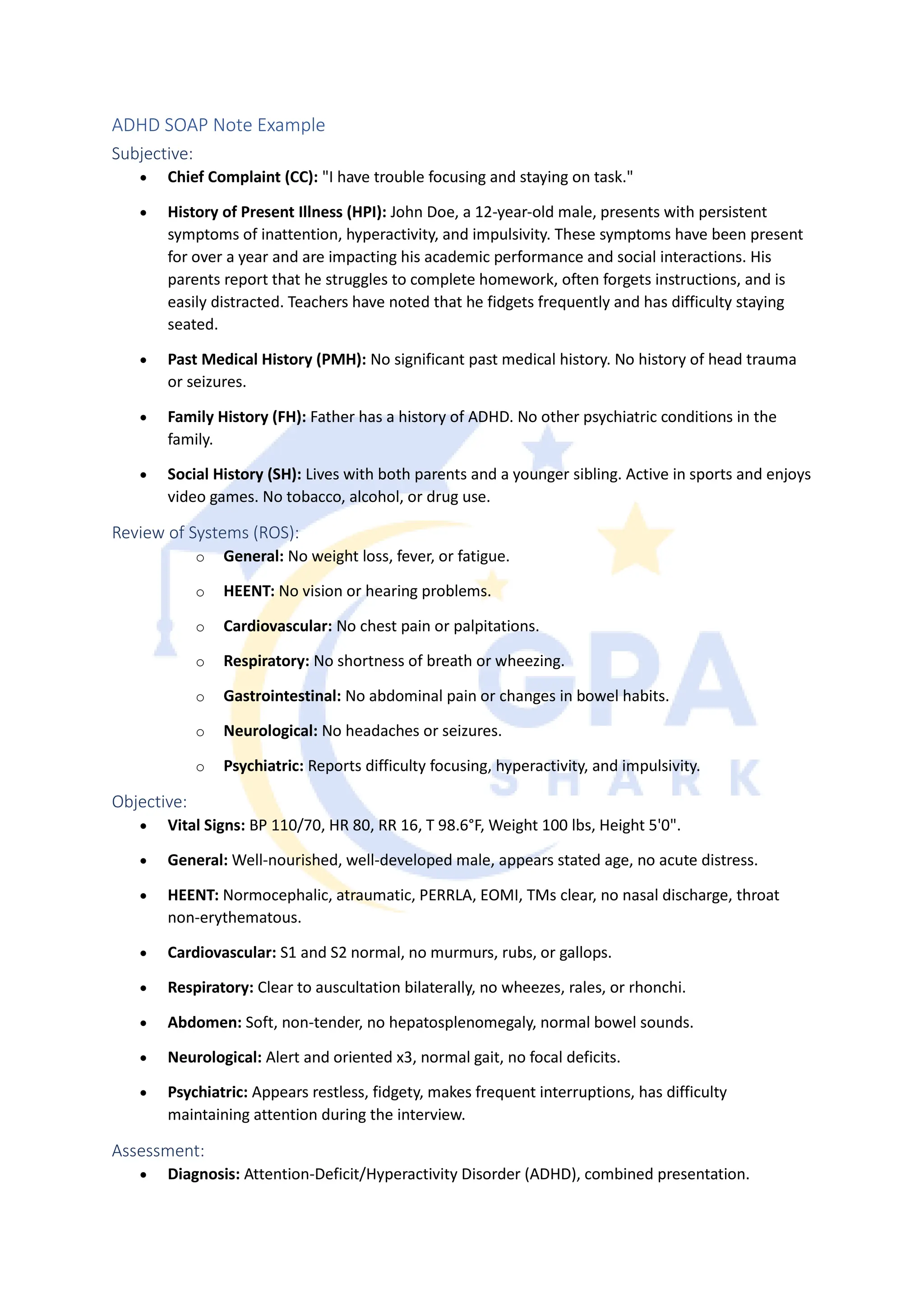
The document provides an example SOAP note for a 12-year-old male patient diagnosed with ADHD, detailing his symptoms, history, and assessments. It includes subjective complaints of inattention and hyperactivity along with an objective examination that shows no significant medical issues. The treatment plan involves medication, behavioral therapy, school accommodations, and parental education, with a follow-up appointment scheduled in four weeks.