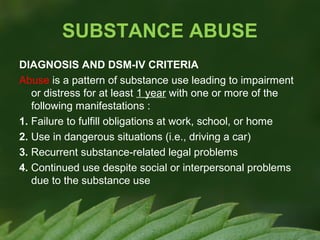
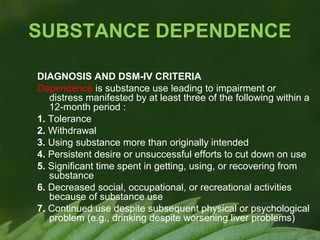
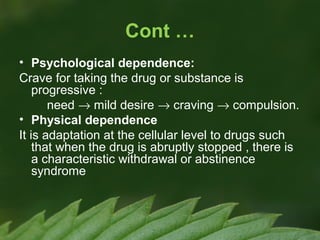
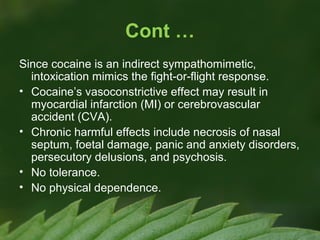
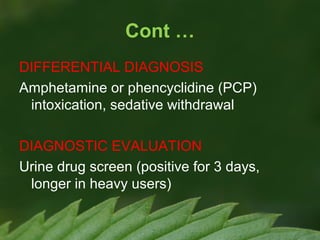
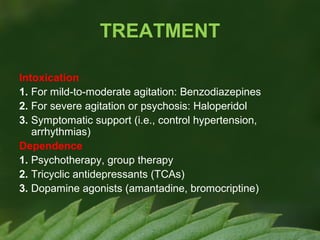
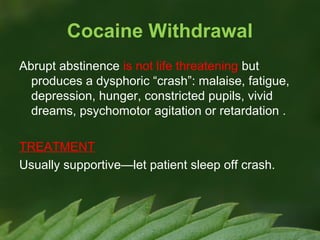
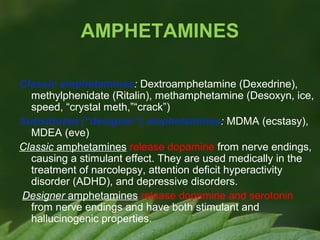
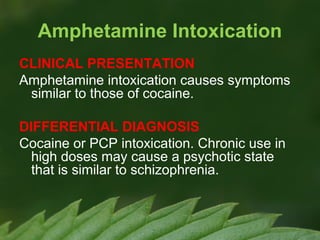
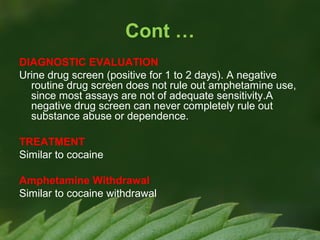
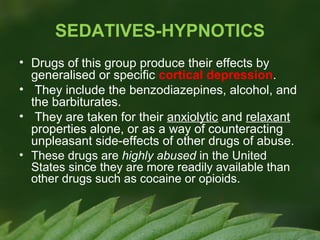
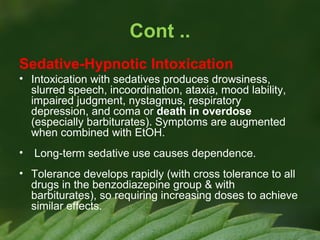
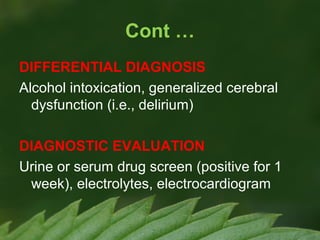
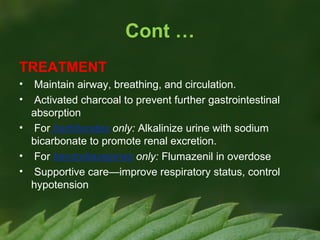
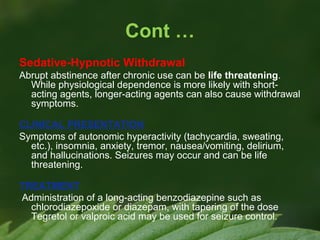
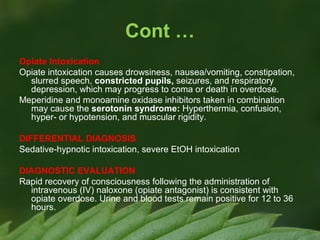
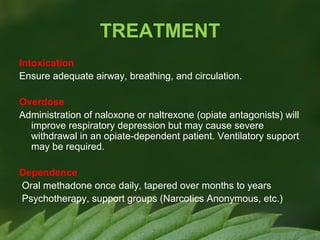
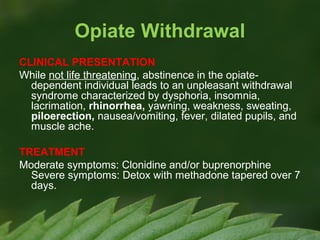
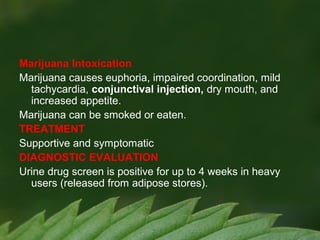
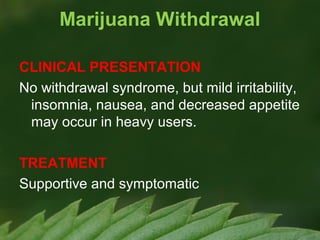
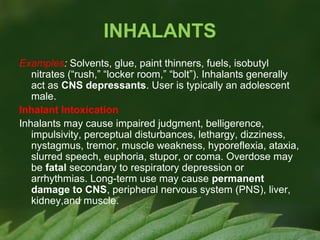
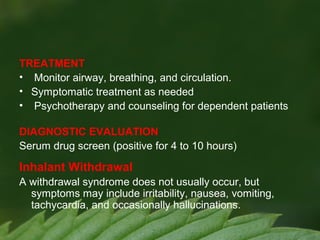
This document provides information on substance-related disorders including substance abuse, dependence, withdrawal, and intoxication. It defines substance abuse and dependence based on DSM-IV criteria. It describes the epidemiology, categories, and effects of commonly abused substances like stimulants, depressants, opiates, hallucinogens, inhalants, and caffeine. For each substance or class, it summarizes intoxication, withdrawal, treatment approaches, and diagnostic evaluation.