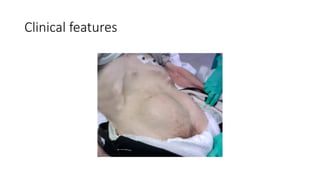
Acute urinary retention is the sudden inability to urinate and is often painful, with potential complications like infection and renal failure. It has a higher incidence in older men, especially those with prostate issues, and requires immediate management through urethral catheterization and addressing underlying causes. Clinical features include acute suprapubic pain, a distended bladder, and the need for paraclinical investigations such as ultrasound and urine culture.