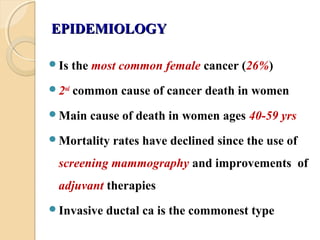
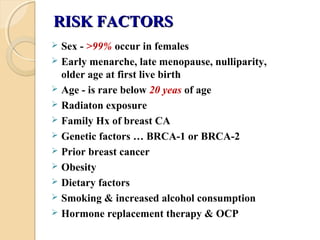
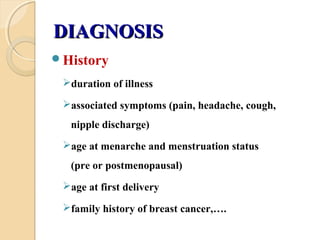
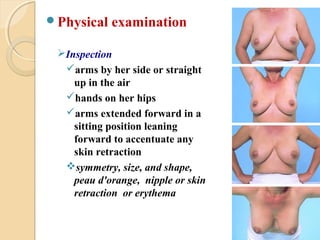
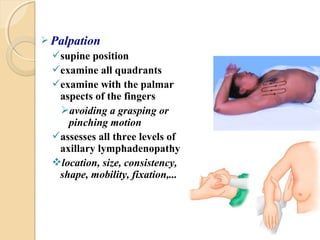
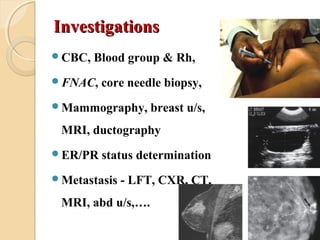
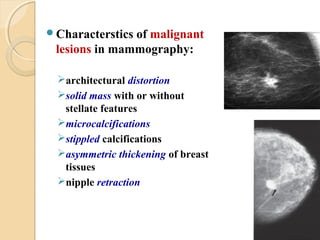
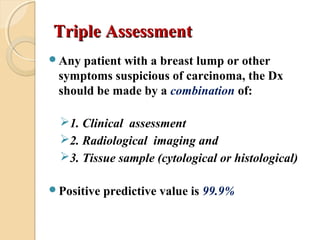
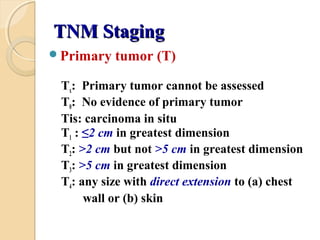
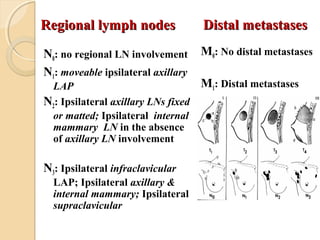
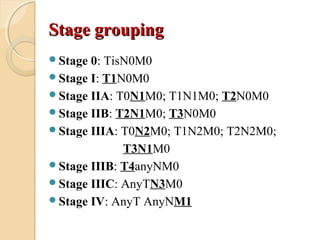
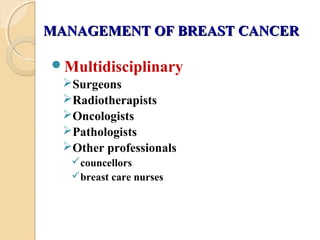
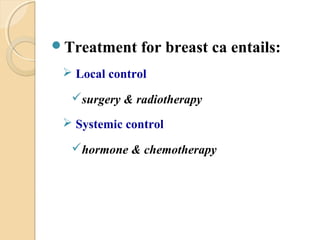
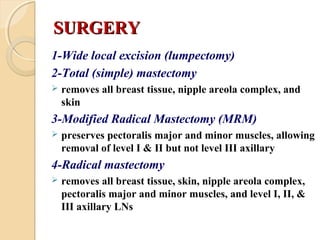
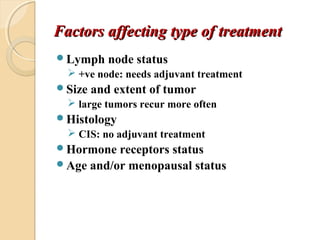
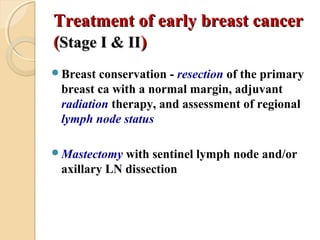
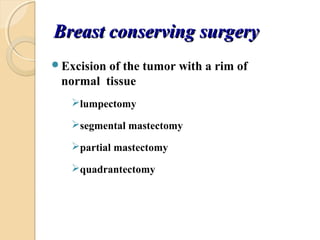
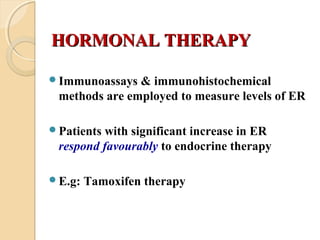
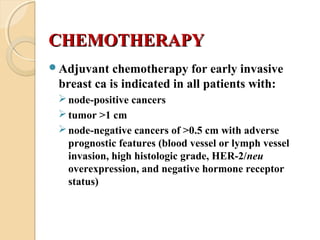
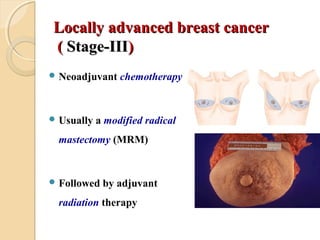
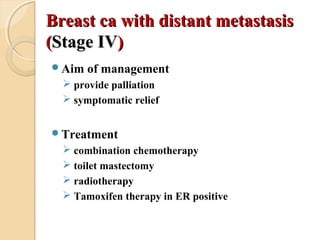
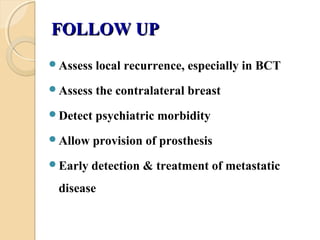
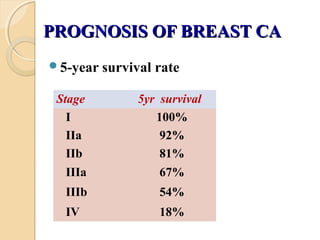
Breast cancer is the most common cancer in women. Risk factors include age, family history, lifestyle factors. Diagnosis involves clinical exam, imaging like mammography, and biopsy. Treatment depends on cancer stage but commonly includes surgery, radiation, hormone therapy and chemotherapy. Prognosis depends on cancer stage and tumor characteristics, with 5-year survival rates ranging from 100% for stage I to 18% for stage IV metastatic cancer.