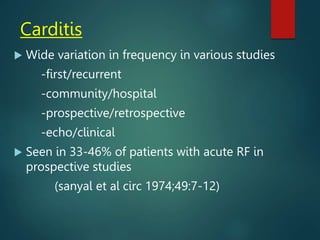
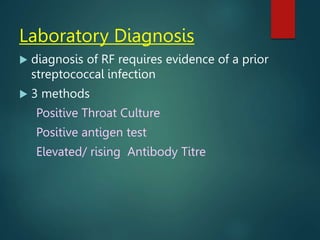
This document discusses rheumatic fever, including its etiology as a delayed complication of streptococcal sore throat, epidemiology showing higher rates in developing countries, pathogenesis involving autoimmune cross-reactivity, and clinical manifestations most commonly involving the heart valves. It provides details on the evolution of the Jones criteria for diagnosis and highlights carditis as the most frequent major manifestation, usually affecting the mitral valve and presenting as mitral regurgitation.



![The Modified Jones Criteria-1956 [Circulation, 1956, 13:
617–620]
MAJOR CRITERIA
Carditis
Polyarthritis
Chorea
Subcutaneous nodules
Erythema marginatum
MINOR CRITERIA
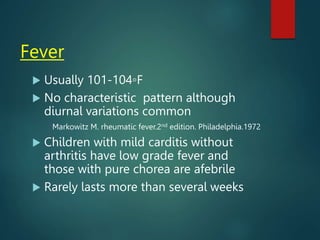
Fever
Arthralgia
Prolonged PR interval
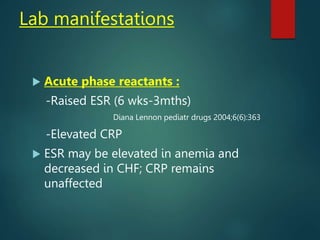
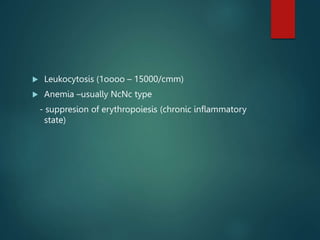
Increased ESR,Leuco-
cytosis,presence of CRP
History of previous
definite ARF or RHD
E/O preceding beta-
hemolytic streptococcal
infection](https://image.slidesharecdn.com/rheumaticfeverfinal-231214041353-af75975e/85/acute-rheumatic-fever-pptx-24-320.jpg)
![The Revised Jones Criteria-1965 [Circulation,
1965, 32:664–668]
MAJOR CRITERIA
Carditis
Polyarthritis
Chorea
Subcutaneous
nodules
Erythema marginatum
MINOR CRITERIA
Fever
Arthralgia
Prolonged PR interval
Increased ESR,
Leucocytosis,presence
of CRP
History of previous
definite ARF or RHD](https://image.slidesharecdn.com/rheumaticfeverfinal-231214041353-af75975e/85/acute-rheumatic-fever-pptx-25-320.jpg)
![The Revised Jones Criteria-1965
Plus supporting evidence of preceding
streptococcal infection: h/o scarlet fever;positive
throat culture for group A streptococcus;increased
ASLO titer or other streptococcal antibodies,
Chorea and chronic carditis [when presenting as
the only major manifestation] were exempted
from this requirement,
The WHO expert committee on rheumatic fever
did not accept the revised criteria as at that time
there were insufficient laboratory facilities in the
developing countries to provide the necessary
supportive evidence.](https://image.slidesharecdn.com/rheumaticfeverfinal-231214041353-af75975e/85/acute-rheumatic-fever-pptx-26-320.jpg)
![The Revised Jones Criteria-1984 [Circulation,1984, 70:204A–
208A]
No major changes,
Avoid premature administration of anti-
inflammatory drugs when s/s are ill-defined,
Role of echo to diagnose MVP
Minor changes: history of a sore throat is not
considered adequate evidence of streptococcal
infection,
Necessity to exclude non-rheumatic causes of
chorea highlighted,
ASLO can be high in non-group-A strep.
infections and strep. skin infections.](https://image.slidesharecdn.com/rheumaticfeverfinal-231214041353-af75975e/85/acute-rheumatic-fever-pptx-27-320.jpg)
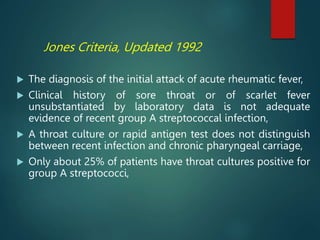
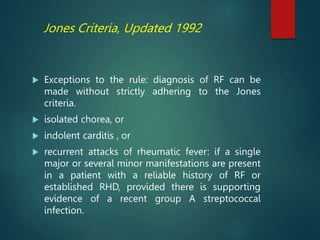
![Jones Criteria, Updated 1992 [JAMA, 1992, 268:2069–
2073]](https://image.slidesharecdn.com/rheumaticfeverfinal-231214041353-af75975e/85/acute-rheumatic-fever-pptx-28-320.jpg)
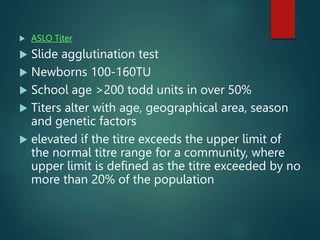
![Jones Criteria, Updated 1992
Rising or elevated streptococcal antibody titer,
A significant antibody increase is usually defined
as a rise in titer of two or more dilution
increments between the acute-phase and
convalescent-phase specimens[2-4 weeks apart],
regardless of the actual height of the antibody
titer,
Extracellular antigens: streptolysin O,
deoxyribonuclease B, nicotinamide adenine
dinucleotidase, hyaluronidase, or streptokinase
The most commonly used antibody assays have
been antistreptolysin O and antistreptokinase,
and more recently anti-deoxyribonuclease B.](https://image.slidesharecdn.com/rheumaticfeverfinal-231214041353-af75975e/85/acute-rheumatic-fever-pptx-30-320.jpg)


![Indian Perspective
Many authors [Roy, Mathur, Cherian etc] have argued that
arthralgia be used as a major criteria in India
These studies were retrospective, did not diff. an initial attack
from recurrences and many patients presented late in the
course of illness when the joint s/s had subsided,
Prospective studies by Sanyal et al [Circulation 1974;49: 7-14]
and Padmavati et al [N Z Med J. 1988 Jun 8;101(847 Pt 2):391-
2] showed that the frequency of polyarthritis in India [67%]
were similar to western data,
Concluded that Jones criteria were applicable equally to
developing countries as well.](https://image.slidesharecdn.com/rheumaticfeverfinal-231214041353-af75975e/85/acute-rheumatic-fever-pptx-34-320.jpg)













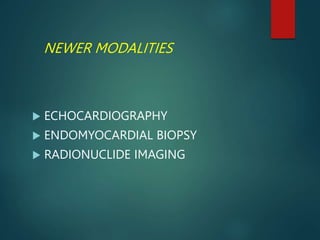
![ECHOCARDIOGRAPHY
ADVANTAGES
More sensitive than routine clinical
auscultation to pick up valvular
regurgitation [esp. with declining
auscultatory skills]
detects subclinical carditis more often and
earlier
Detects valve structure and excludes non-
rheumatic causes [MVP,BAV, innocent
murmurs]](https://image.slidesharecdn.com/rheumaticfeverfinal-231214041353-af75975e/85/acute-rheumatic-fever-pptx-99-320.jpg)
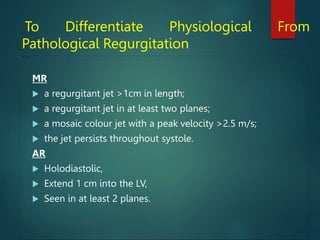
![ ECHO equivalents of verrucae -3-5 mm size focal
nodular thickening situated on tips and bodies
of leaflets, having a different echogenecity , no
bizarre motion of a vegetation, and tending to
disappear on follow up
Mechanism of MR
• Valvular thickening
• Leaflet prolapse [esp AML]
• Annular dilatation/Vent enlargement
• rupture of chordae](https://image.slidesharecdn.com/rheumaticfeverfinal-231214041353-af75975e/85/acute-rheumatic-fever-pptx-100-320.jpg)



![Figueroa FE et al.Heart, 2001, 85:407–410.
35 patients of RF evaluated clinically and by echo,
32 pts at 1 year and 17 pts at 5 years,
15 patients had carditis clinically at admission,
At admission, MR/AR by Doppler found in 25/35
patients vs. 5/35 by clinical exam
10 [30%] of 20 patients of ARF WITHOUT carditis
had doppler e/o regurgitation but no murmur.
These were taken as subclinical carditis,
3 of the subclinical and 3 of the clinical carditis
still had the lesions at 5 years](https://image.slidesharecdn.com/rheumaticfeverfinal-231214041353-af75975e/85/acute-rheumatic-fever-pptx-106-320.jpg)
![ECHOCARDIOGRAPHY
DISADVANTAGES
Availability restricted
Will not detect recurrences unless previous echo
data available to satisfy interval change
physiological valvular regurgitation in normal
people : MR 2.4–45% , AR in 0–33% ,TR in 6.3–
95% ,and PR in 21.9–92% of normal individuals
[WHO Technical Report Series 923]
Management of subclinical carditis will not
change.The data of benign prognosis in patients
without carditis have essentially come from
clinical studies.](https://image.slidesharecdn.com/rheumaticfeverfinal-231214041353-af75975e/85/acute-rheumatic-fever-pptx-110-320.jpg)
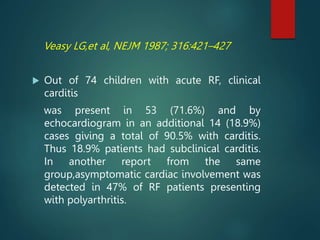
![Narula J et al. Circulation, 1993, 88:2198–2205.
RV Em Bx in 54 pts of clinical RF and quiescent RHD
Interstitial inflammation that ranged from perivascular
mononuclear cellular infiltration, to histiocytic aggregates and
Aschoff nodule formation.
myocarditis was virtually absent as defined by the Dallas
criteria [only one specimen].
Concluded
Endomyocardial biopsy does not provide additional
diagnostic information where clinical consensus is certain
about diagnosis of carditis
cannot recommend endomyocardial biopsy as a routine
diagnostic or prognostic tool](https://image.slidesharecdn.com/rheumaticfeverfinal-231214041353-af75975e/85/acute-rheumatic-fever-pptx-113-320.jpg)
![RADIONUCLIDE IMAGING
1. Gallium-67 imaging
2. Leukocytes labelled with Indium-111 or
technetium-99m
3. In-111-labeled antimyosin antibodies
Gallium-67 imaging most promising
[Sensitivity 86 %, specificity 100%]
Superior to antimyosin antibody imaging
Insufficient data and not enough experience
with such methods to allow them to be used
for the routine diagnosis](https://image.slidesharecdn.com/rheumaticfeverfinal-231214041353-af75975e/85/acute-rheumatic-fever-pptx-114-320.jpg)