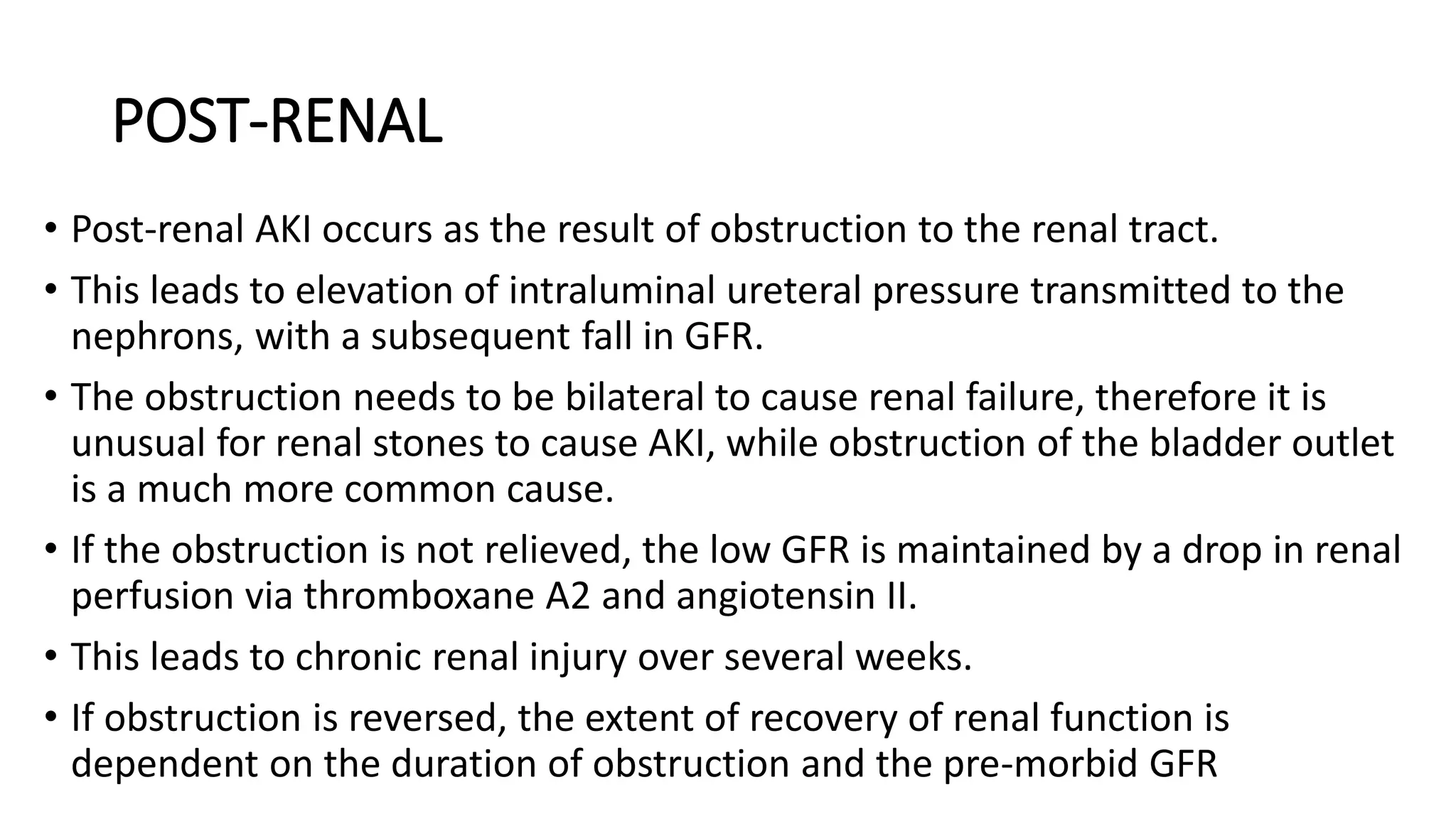
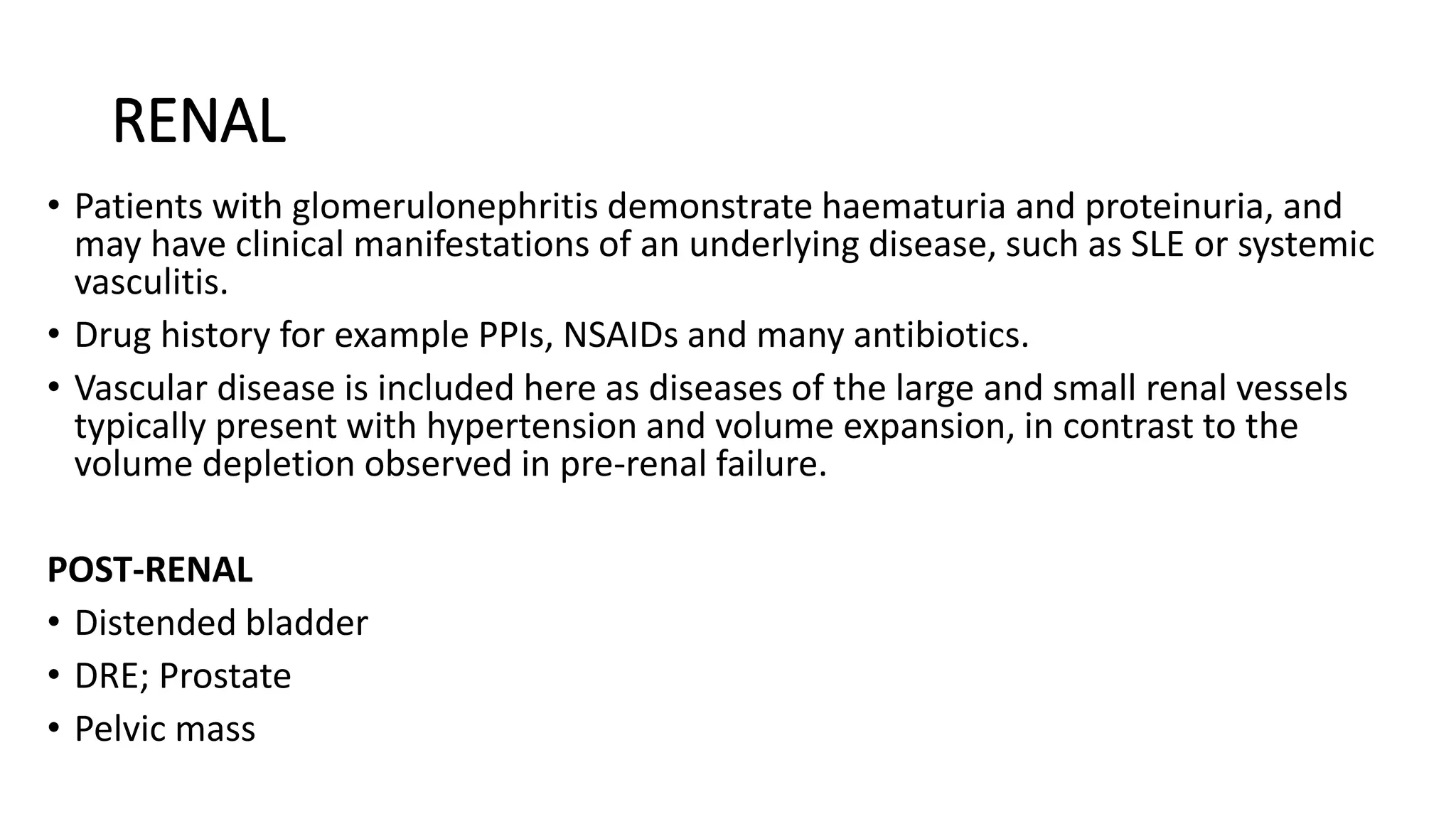
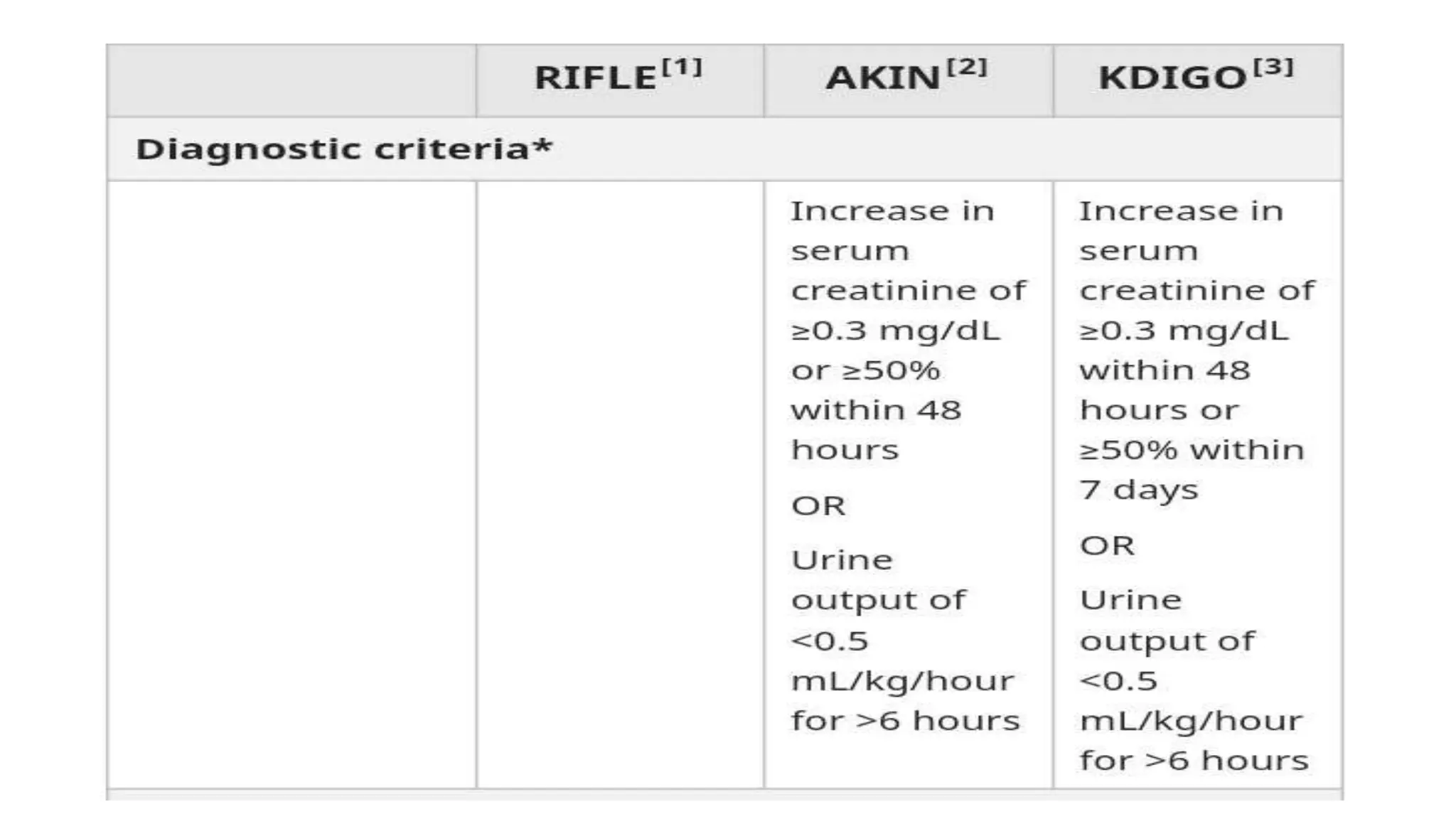
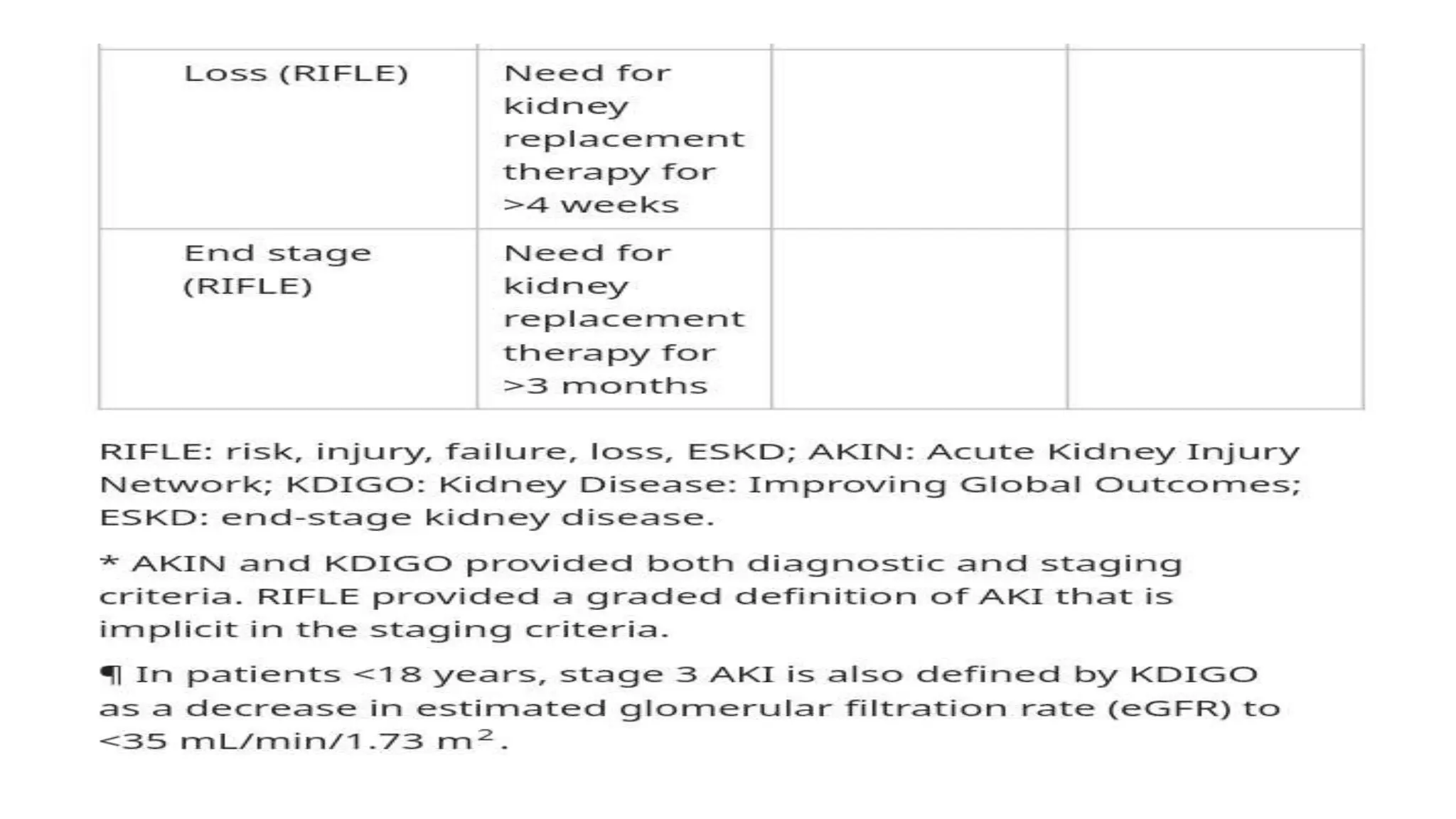
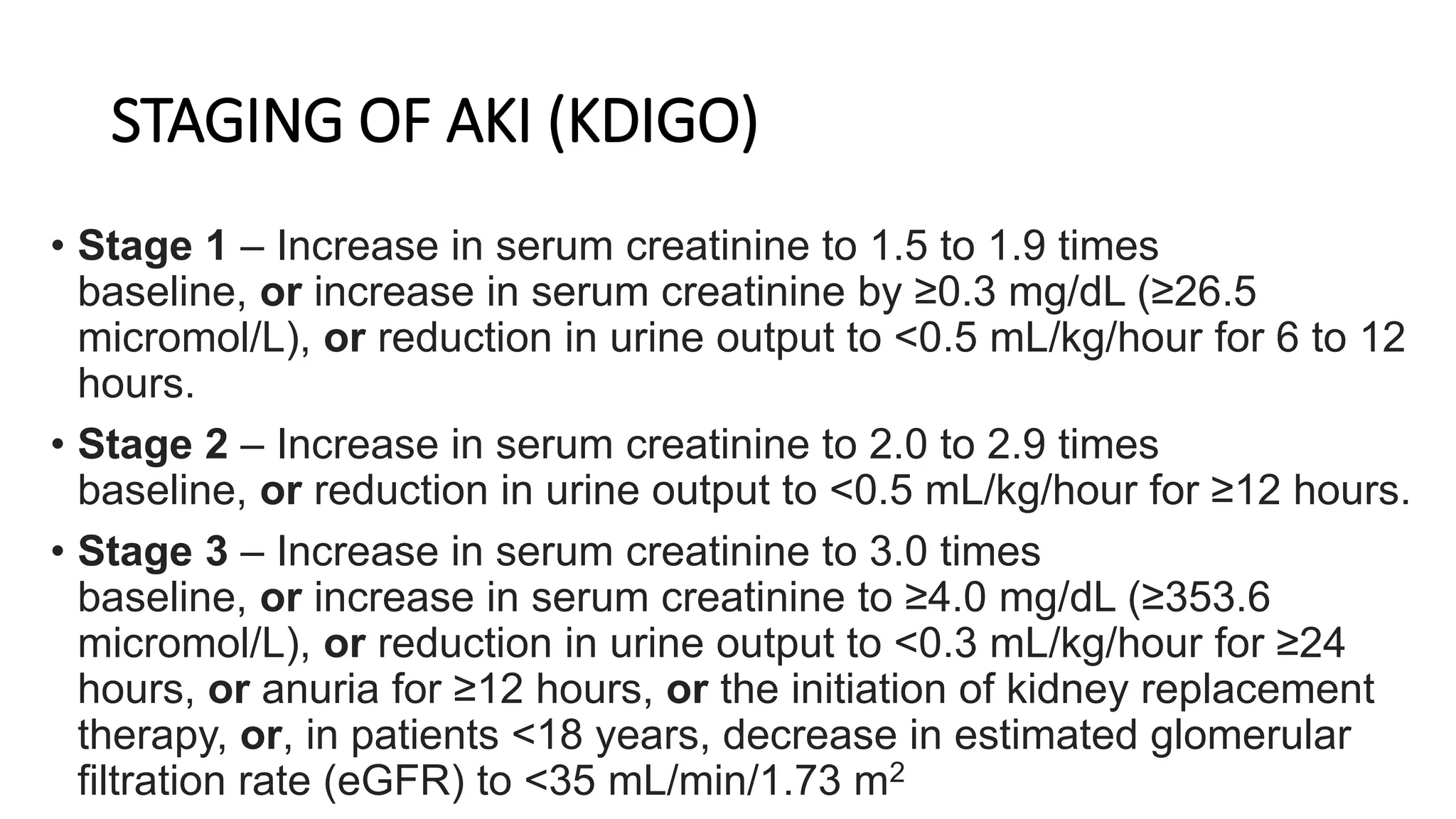
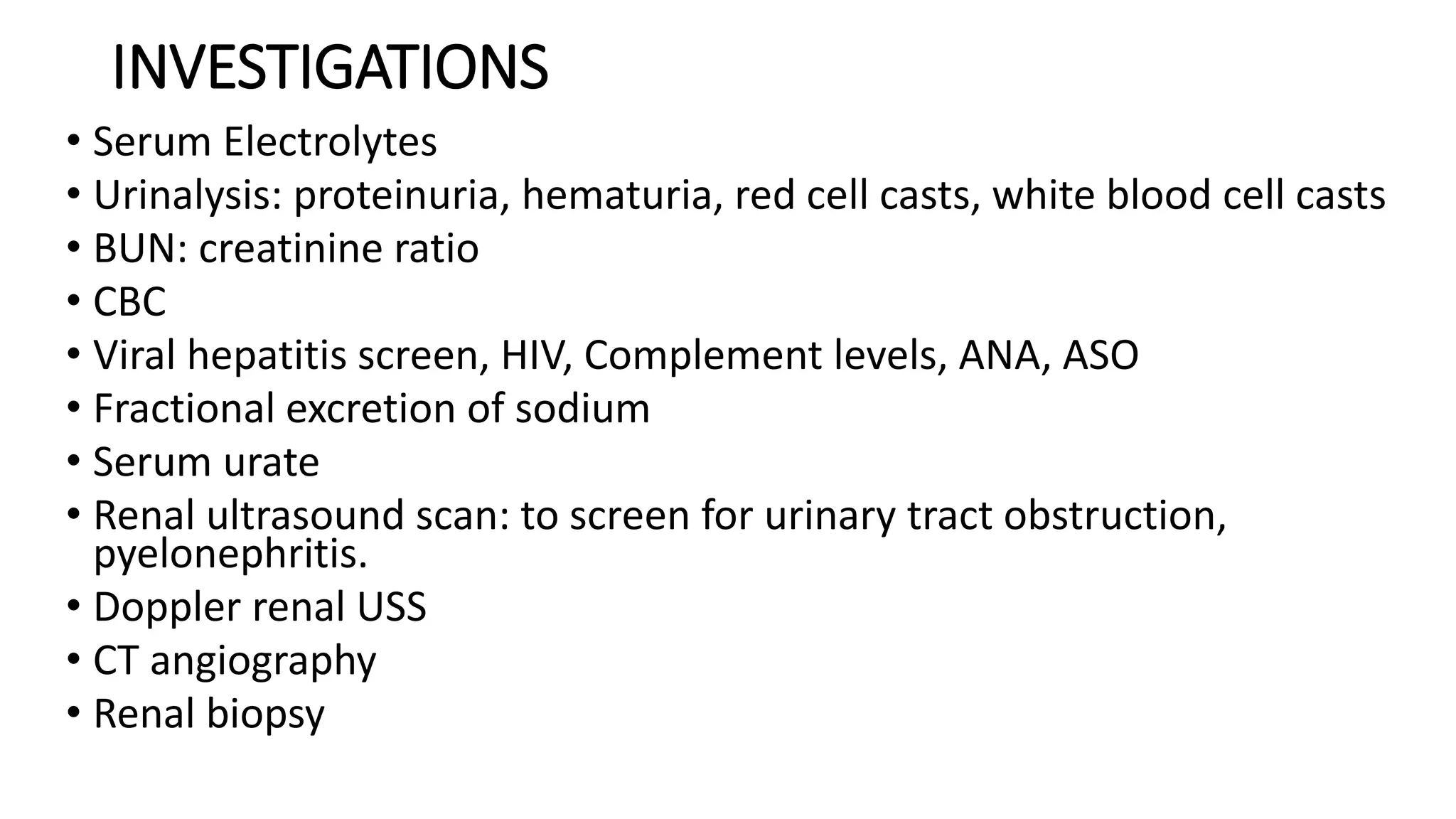
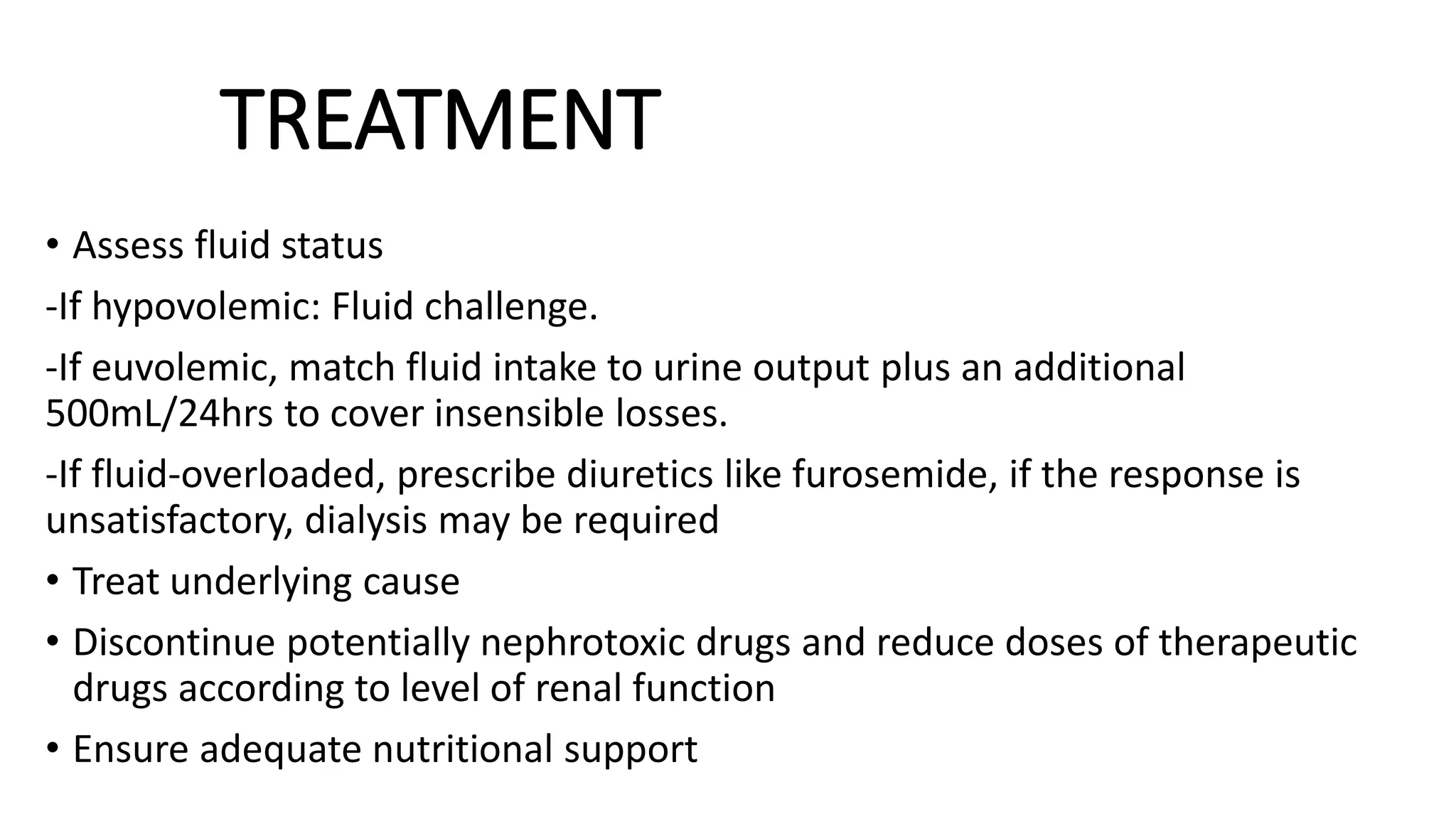
This document provides an overview of acute kidney injury (AKI). It defines AKI and notes its worldwide epidemiology. The main causes of AKI are discussed as pre-renal, renal, and post-renal. The pathophysiology of each type is explained. Clinical presentation depends on the cause but may include elevated creatinine and reduced urine output. Staging of AKI is outlined using KDIGO criteria. Investigations and management aim to identify and treat the underlying cause while maintaining fluid and electrolyte balance. Complications include fluid overload and metabolic disturbances. Prognosis depends on severity and comorbidities.