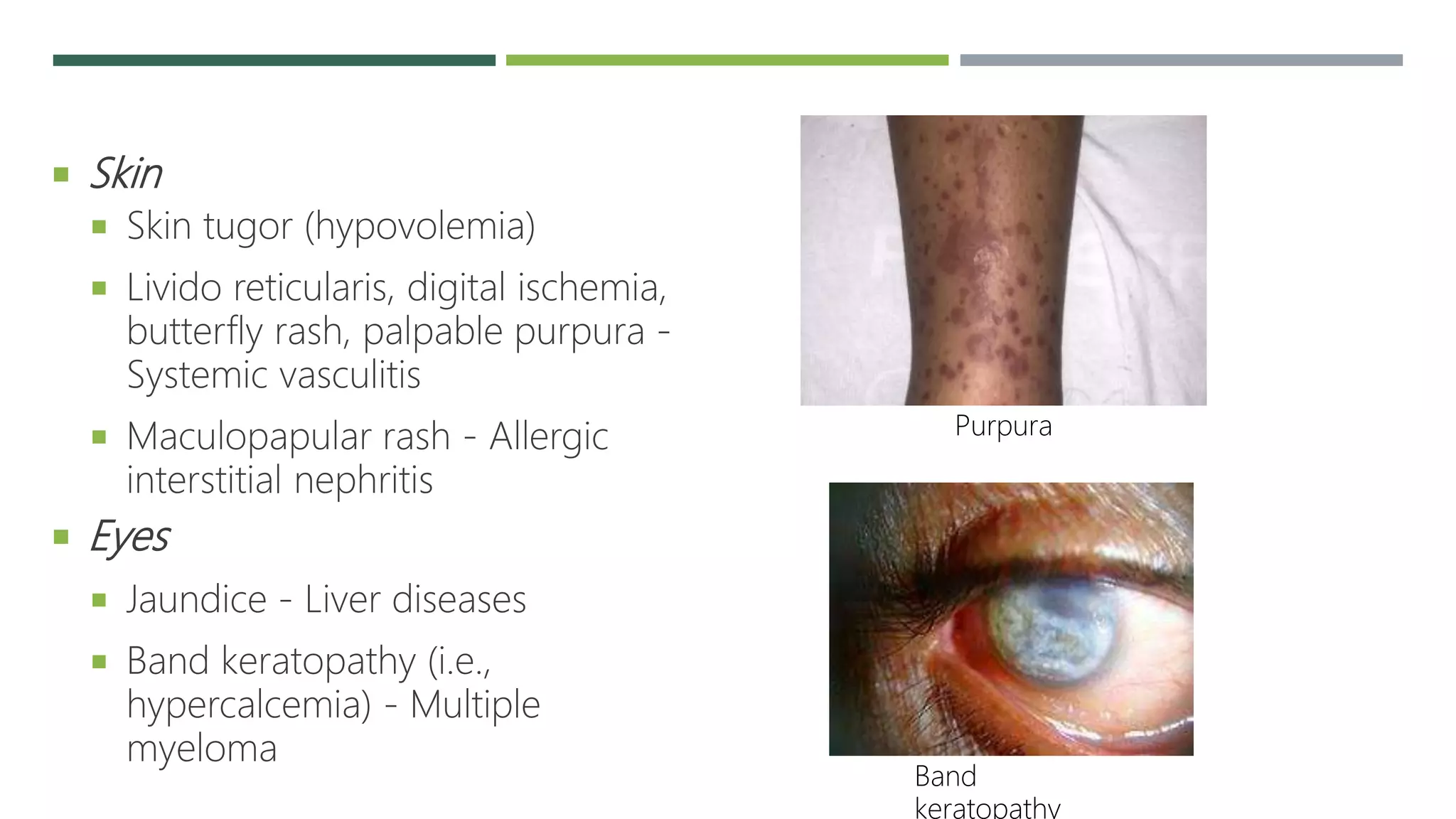
This document presents a case of acute kidney injury (AKI) in a 74-year-old male farmer who presented with reduced urine output. It provides details on his medical history, examination, initial workup and assessment of AKI likely due to toxic nephropathy, dehydration and possible sepsis. The document then provides an introduction to AKI including definitions, epidemiology, etiology and pathophysiology involving pre-renal, intrinsic and post-renal causes. It also discusses approaches to assessing patients with AKI including history, physical examination and investigations.
























































![REFERENCE
Harrison’s principle of Internal Medicine
Oxford handbook of internal medicine
Schrier RW, Wang W, Poole B, Mitra A. Acute renal failure: definitions, diagnosis,
pathogenesis, and therapy. J Clin Invest. 2004 Jul. 114(1):5-14. [QxMD MEDLINE
Link]. [Full Text].
Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, et al. Acute Kidney
Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit
Care. 2007. 11(2):R31. [QxMD MEDLINE Link]. [Full Text].
Ricci Z, Cruz D, Ronco C. The RIFLE criteria and mortality in acute kidney injury: A
systematic review. Kidney Int. 2008 Mar. 73(5):538-46. [QxMD MEDLINE Link].](https://image.slidesharecdn.com/acutekidneyinjury-220601205412-dd435226/75/ACUTE-KIDNEY-INJURY-pptx-59-2048.jpg)
