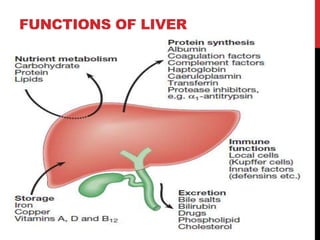
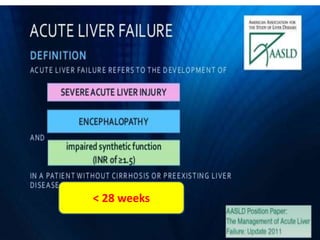
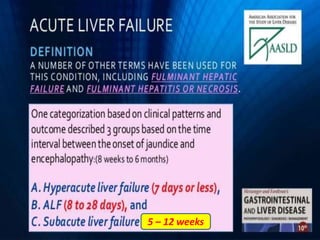
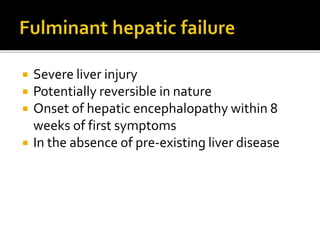
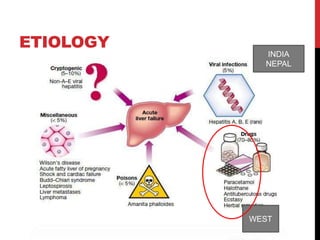
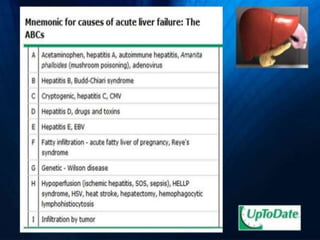
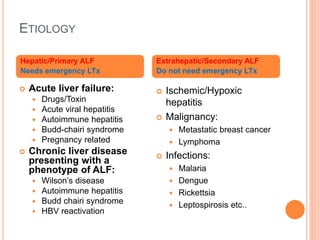
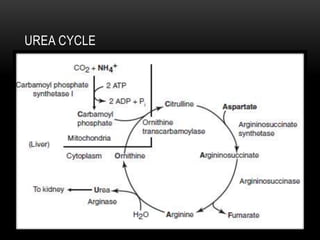
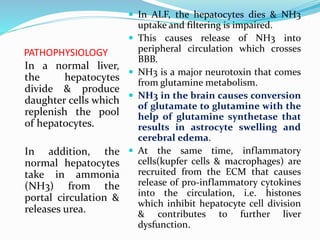
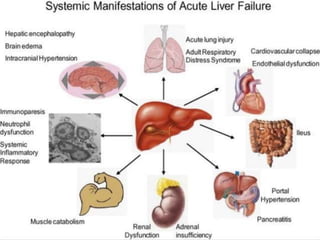
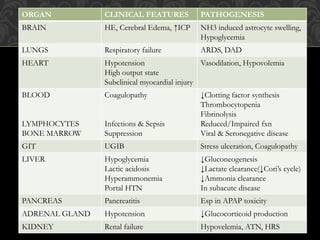
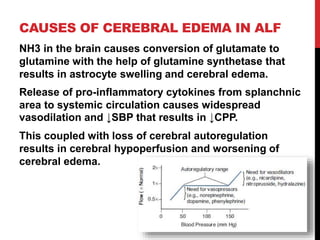
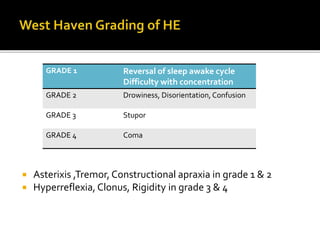
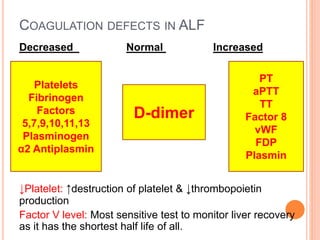
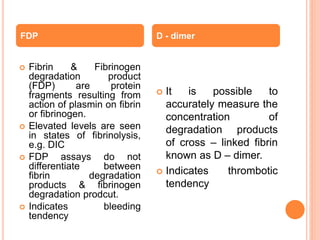
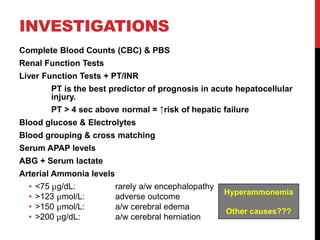
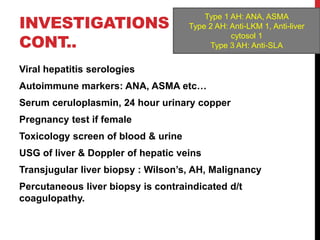
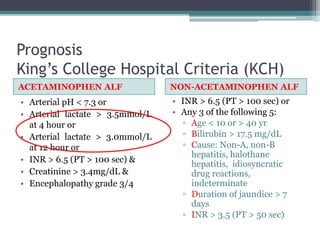
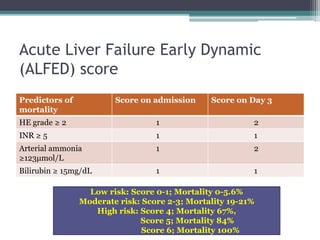
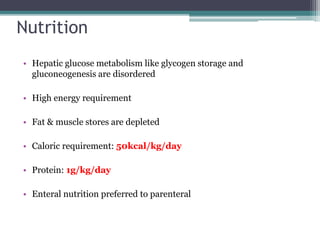
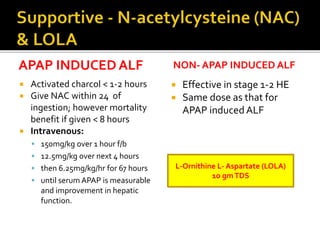
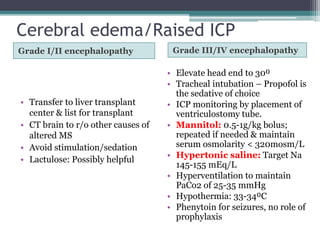
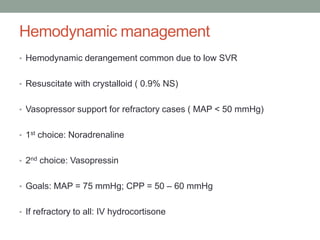
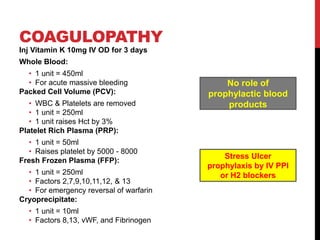
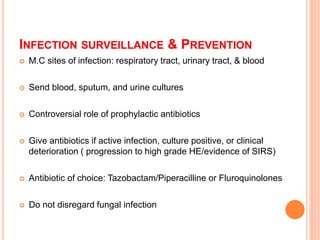
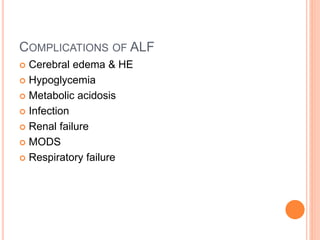
This document provides information about acute liver failure (ALF), including its definition, etiology, pathophysiology, clinical features, investigations, prognosis, and management. ALF is characterized by severe liver injury and encephalopathy within 8 weeks without pre-existing liver disease. Common causes include drugs/toxins, viral hepatitis, and autoimmune conditions. In ALF, liver cells die rapidly, impairing ammonia clearance and coagulation factor production, which can lead to cerebral edema, coagulopathy, and multi-organ failure without transplantation. Prognosis is assessed using tools like KCH or ALFED scores. Management involves supportive care, treating the underlying cause, and considering transplantation for eligible patients.