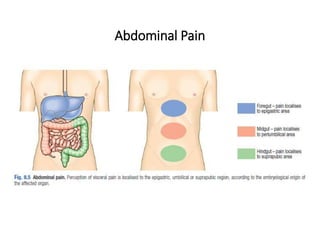
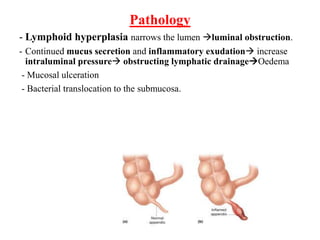
1. Acute appendicitis is a common condition that usually presents with abdominal pain that starts around the navel and shifts to the lower right abdomen. Other common symptoms include anorexia, nausea, and vomiting.
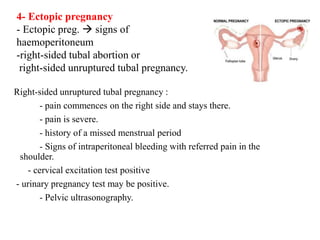
2. A clinical examination often reveals tenderness at McBurney's point with guarding and rebound tenderness. Special tests like Rovsing's sign may also indicate appendicitis. Differential diagnoses include other abdominal conditions.
3. The diagnosis is usually made based on history and clinical exam findings. Laboratory tests are not usually required but may include a CBC and urinalysis. Imaging tests like ultrasound or CT scans can help in unclear cases. Prompt diagnosis and treatment is important to