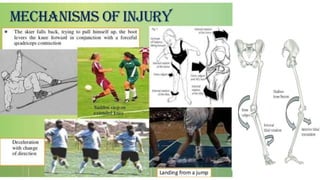
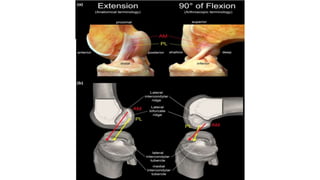
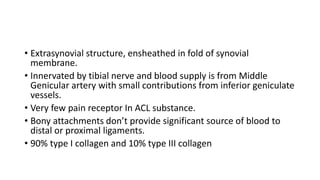
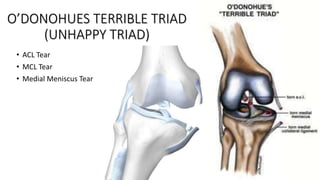
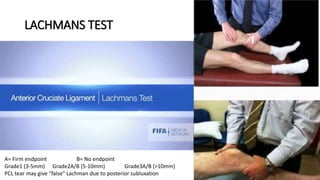
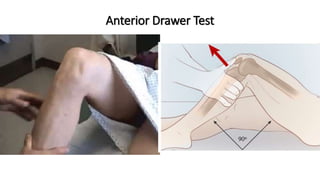
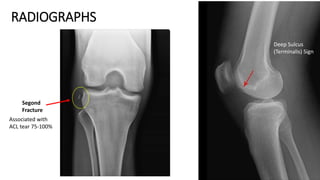
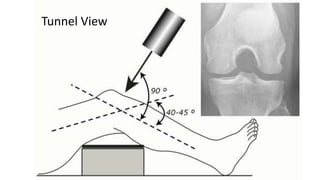
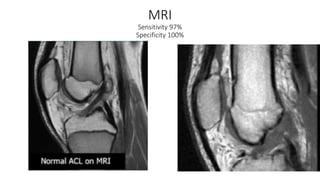
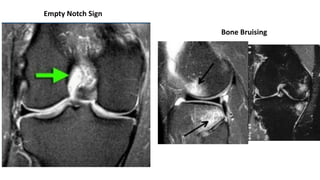
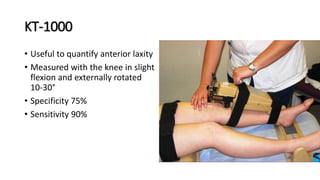
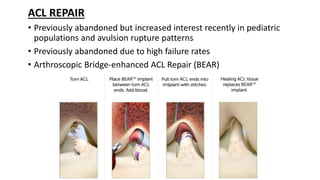
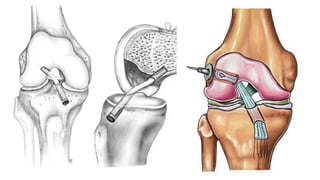
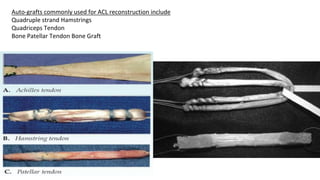
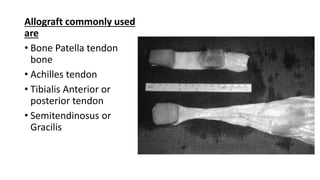
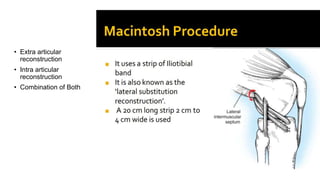
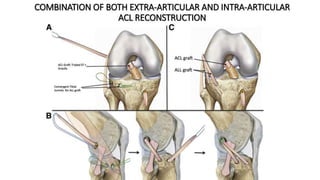
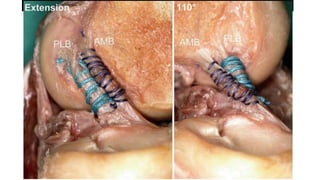
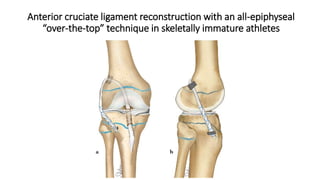
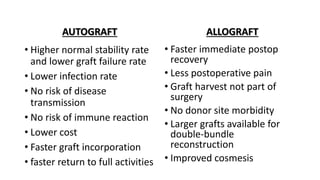
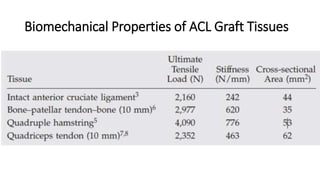
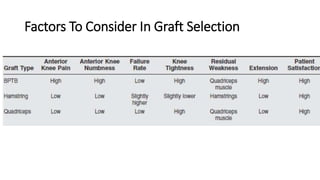
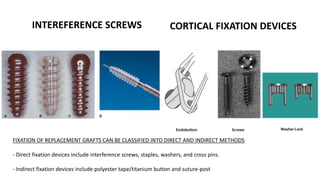
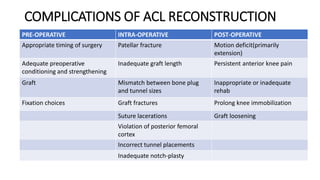
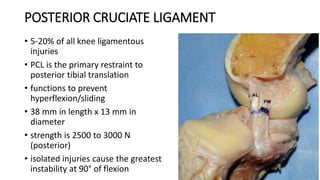
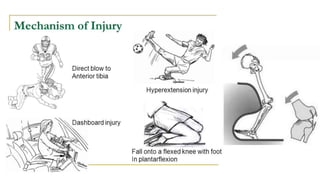
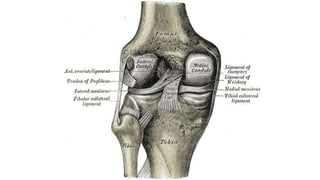
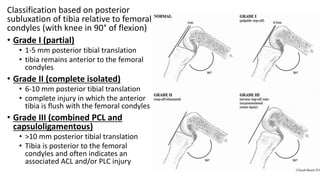
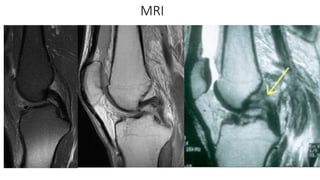
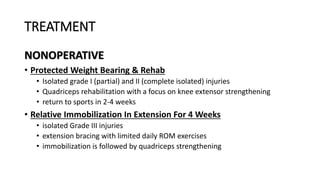
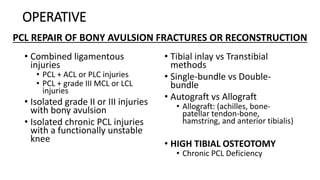
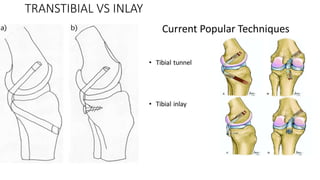
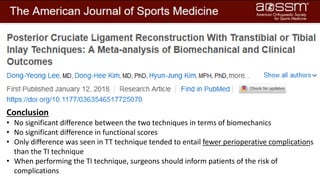
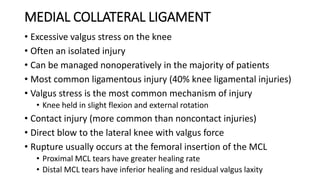
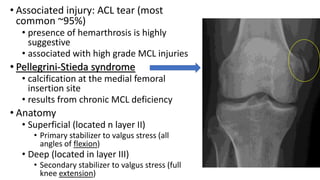
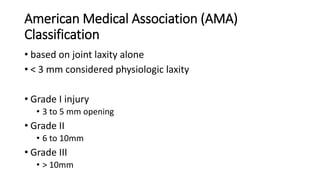
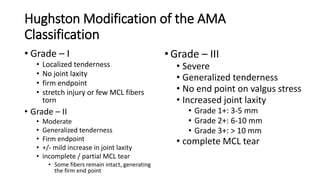
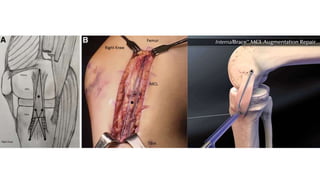
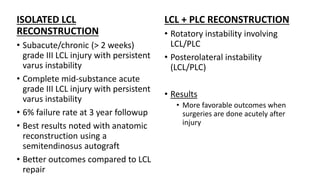
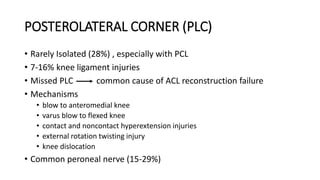
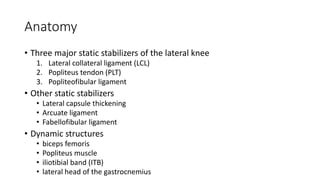
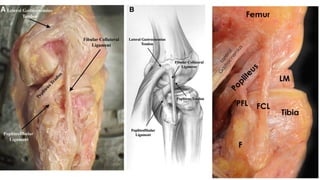
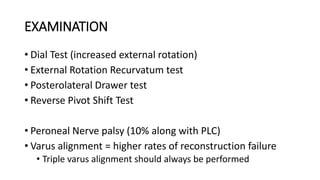
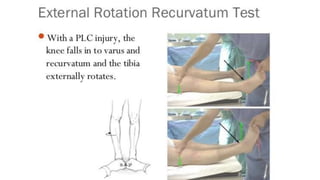
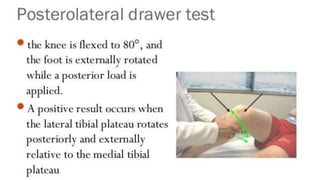
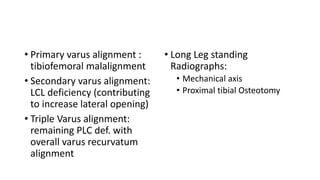
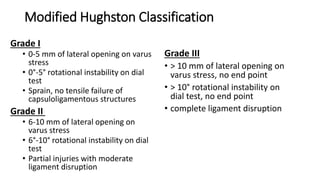
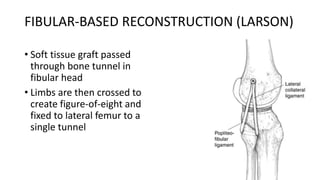
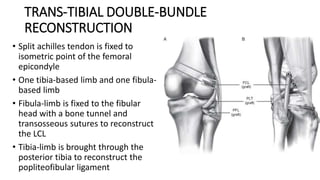
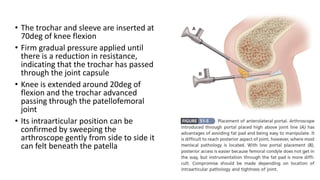
This document summarizes information about soft tissue injuries of the knee joint, focusing on injuries to the anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL). It describes the anatomy, biomechanics, classification systems, clinical presentations, diagnostic tests, and treatment options for ACL and PCL injuries. It also briefly discusses medial collateral ligament (MCL) injuries and provides comparisons of surgical reconstruction techniques for ACL and PCL injuries.