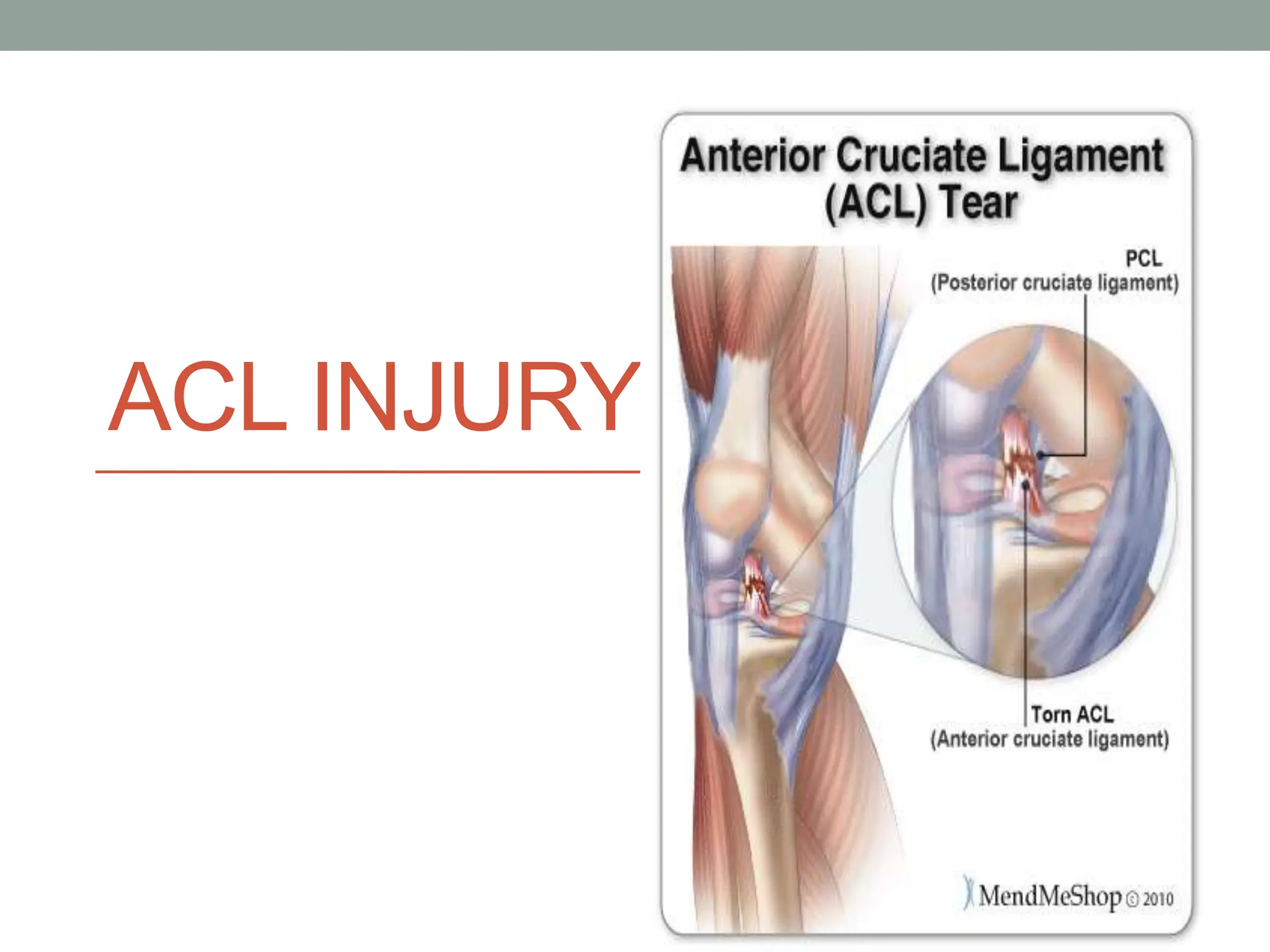
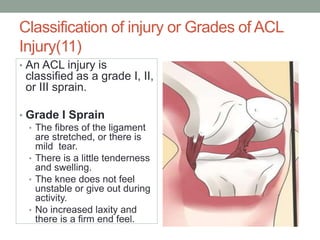
- Injuries to the anterior cruciate ligament (ACL) are common in sports requiring pivoting movements and can range from mild sprains to complete tears.
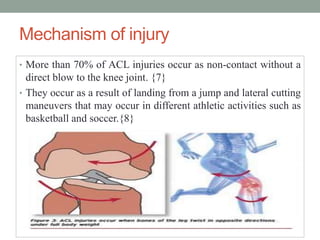
- Mechanisms of ACL injury often involve sudden deceleration, landing from a jump with the knee in valgus, or lateral cutting maneuvers without contact.
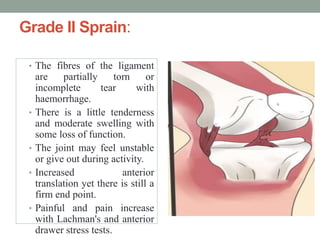
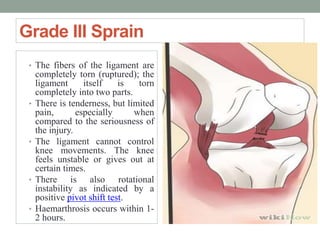
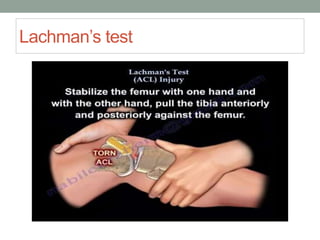
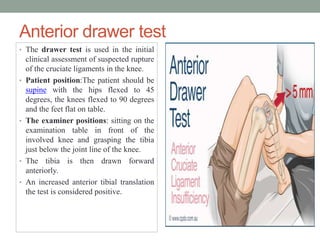
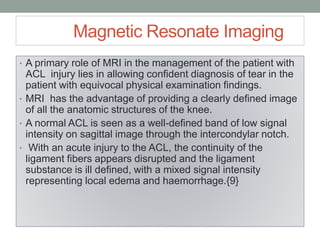
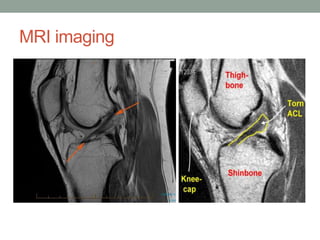
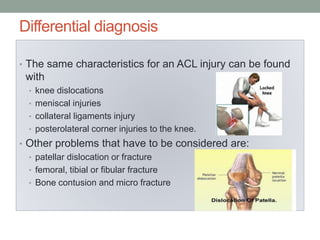
- Diagnosis involves clinical exam including Lachman's and anterior drawer tests along with imaging like MRI to visualize ligament integrity.
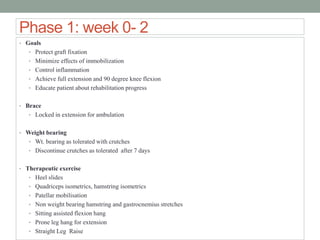
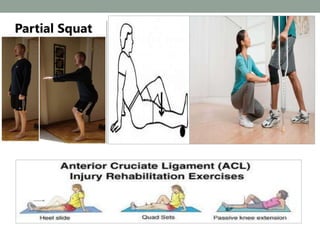
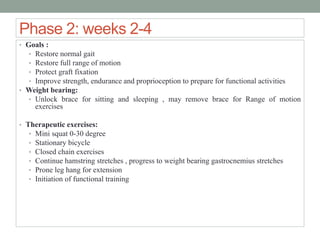
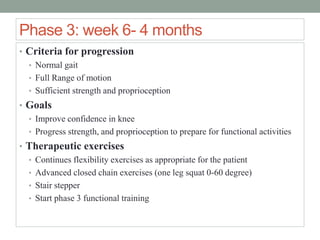
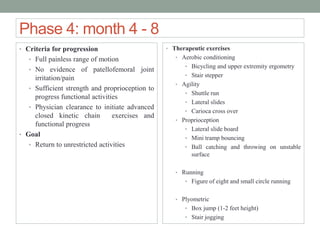
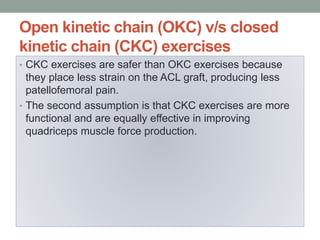
- Treatment options include rehabilitation for mild injuries or reconstruction surgery followed by lengthy physical therapy focusing on regaining range of motion and strength.