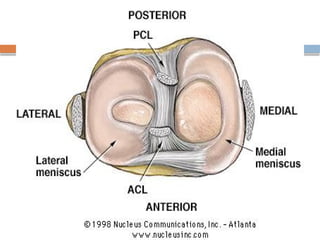
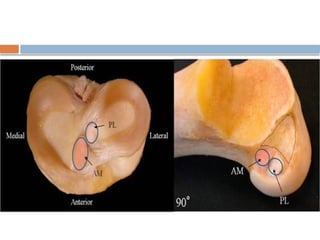
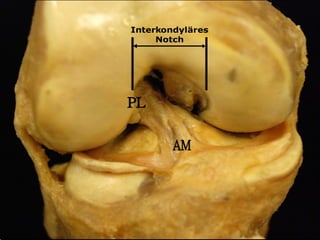
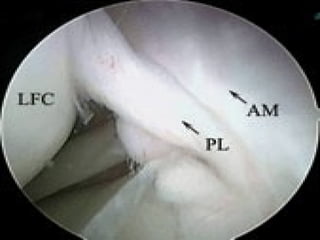
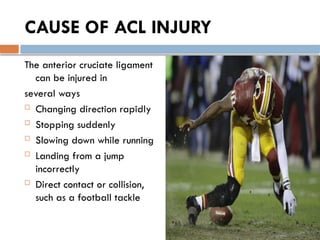
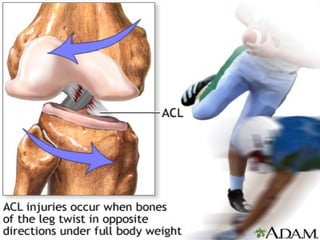
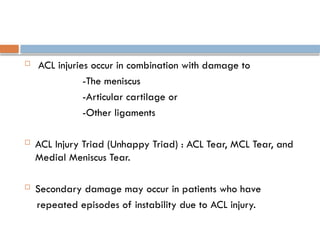
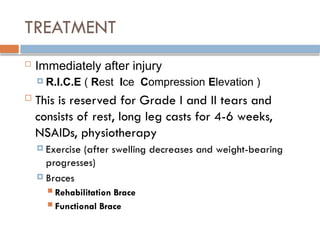
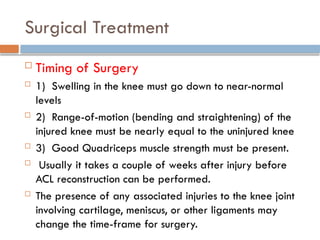
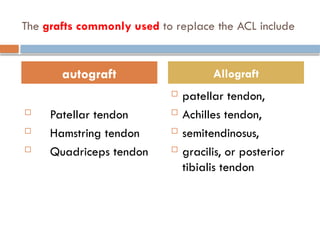
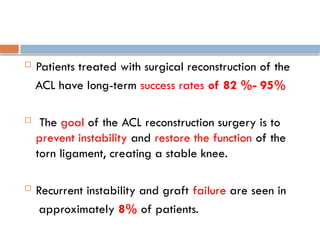
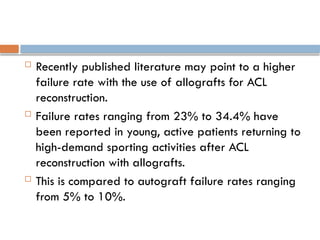
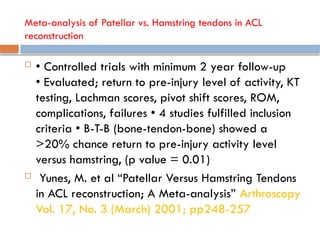
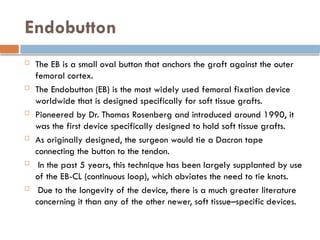
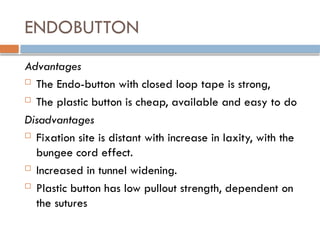
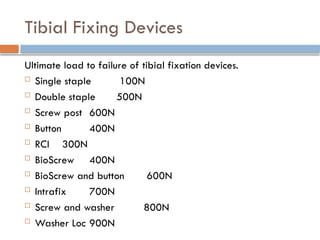
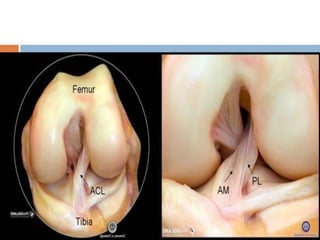
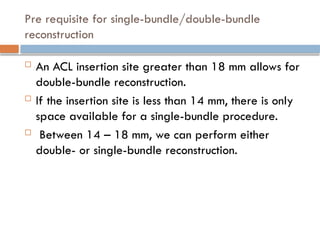
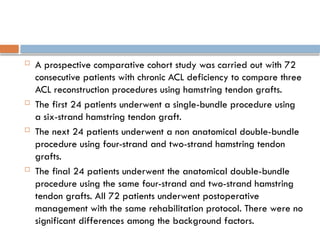
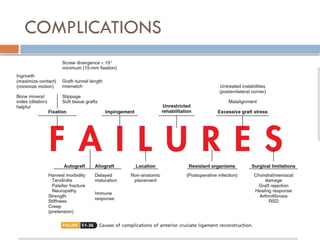
The document provides a comprehensive overview of the anatomy, injury mechanisms, clinical implications, symptoms, and management strategies for anterior cruciate ligament (ACL) injuries. It discusses detailed classification, diagnostic tests, and both non-surgical and surgical treatment options including various graft types used for reconstruction, with emphasis on their advantages and disadvantages. Additionally, it addresses the differences in injury rates between males and females and outlines the importance of considering patient activity levels and associated injuries when determining treatment approaches.