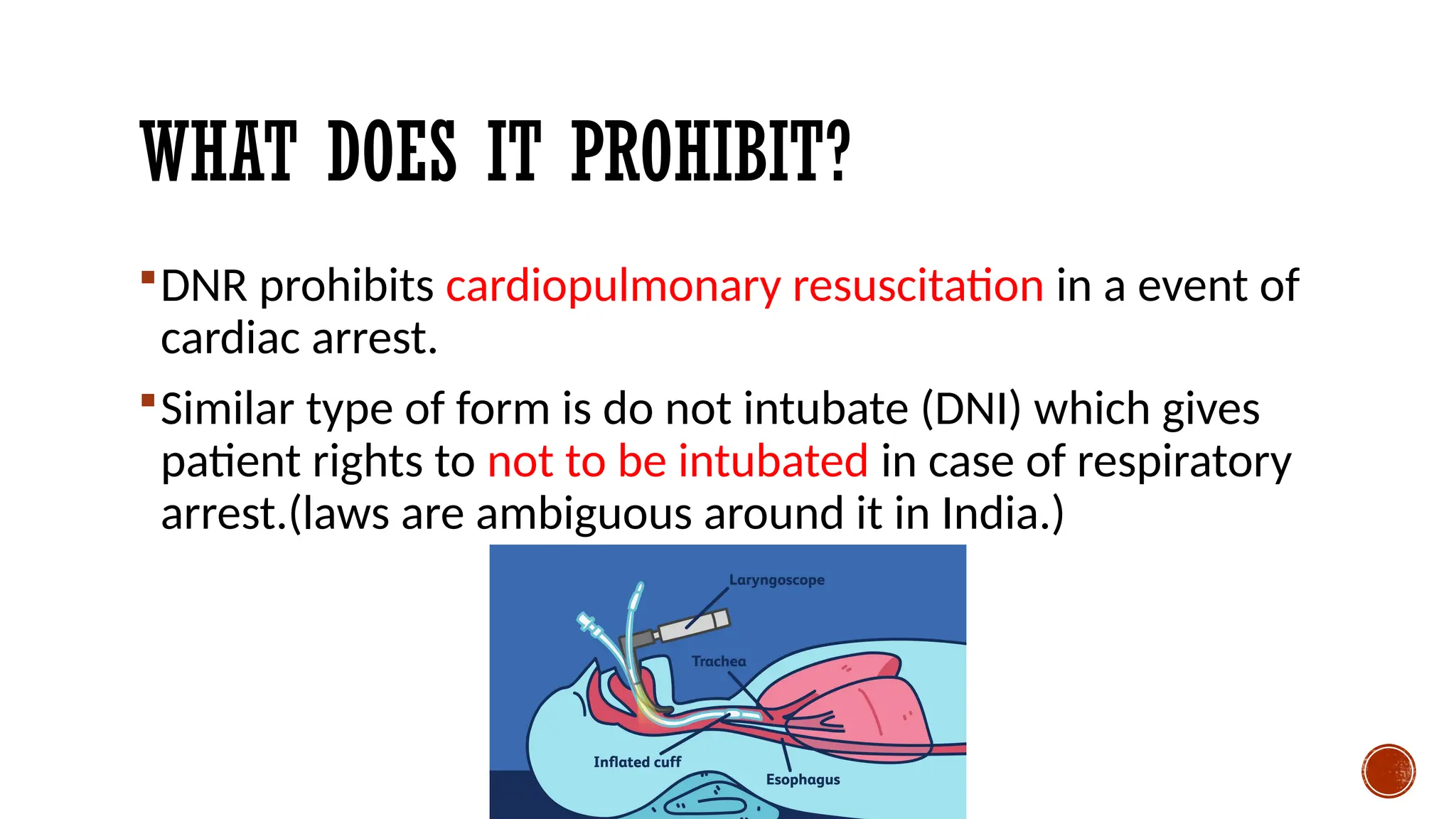
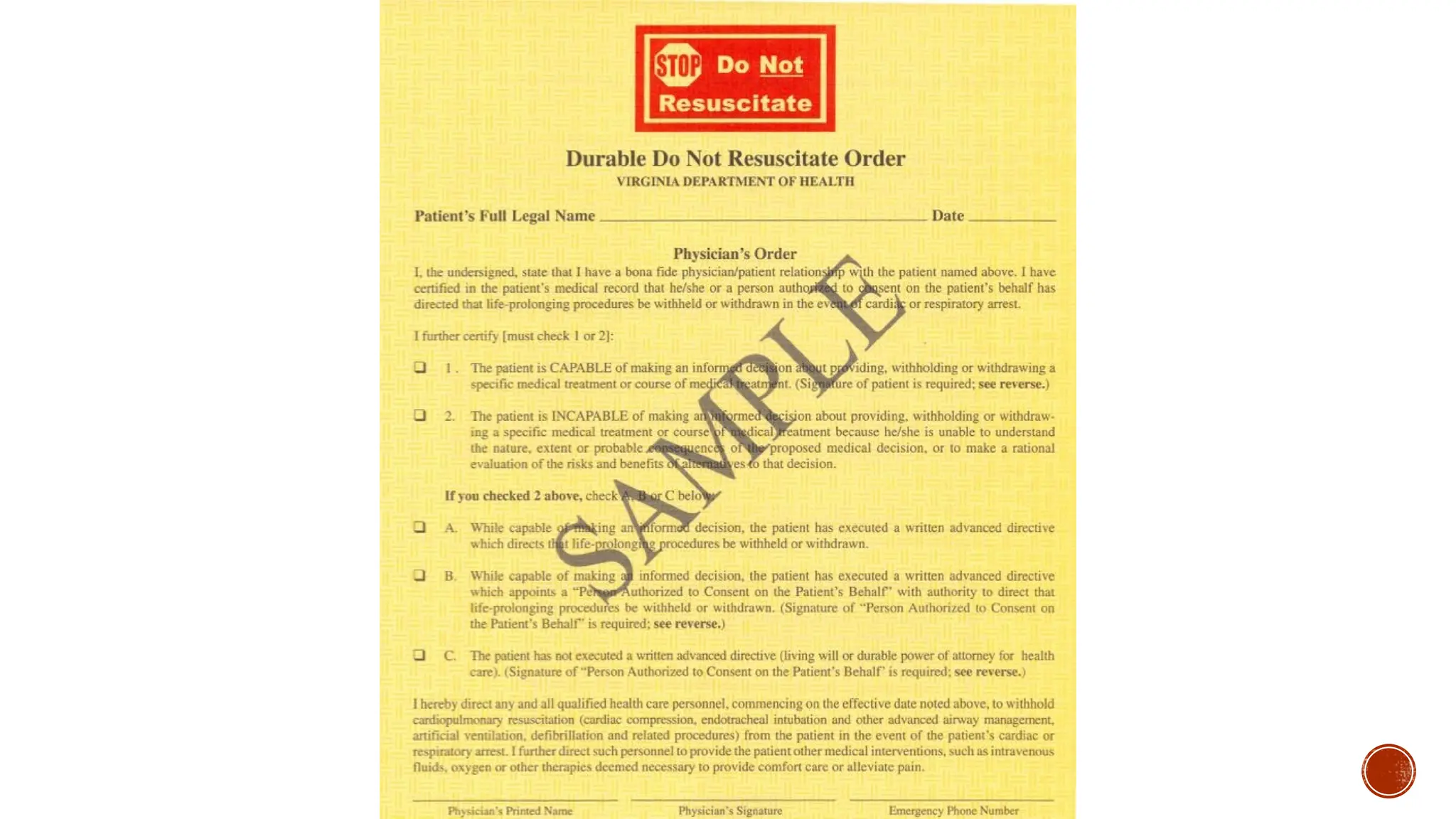
The document discusses do not resuscitate (DNR) orders, which allow patients to decline life-saving treatments in favor of natural death if they are seriously ill and unable to express their wishes. It outlines the ethical and legal considerations in making DNR decisions, emphasizing communication and documentation among healthcare providers, patients, and their surrogates. Overall, it highlights the importance of respecting patient autonomy and ensuring the decision-making process is well-supported and clear.