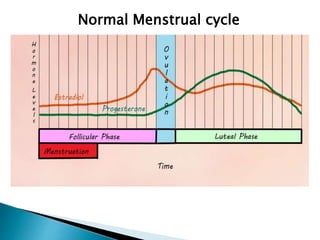
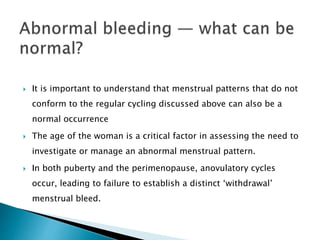
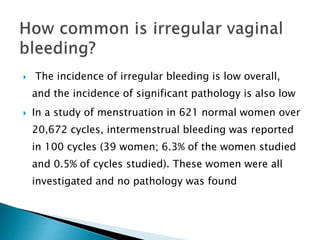
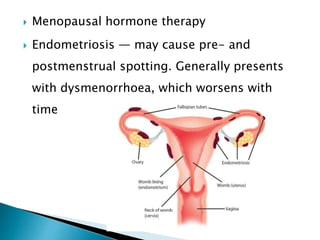
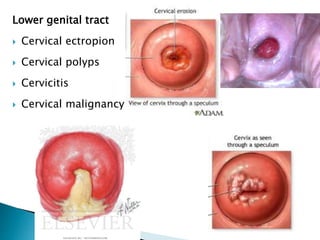
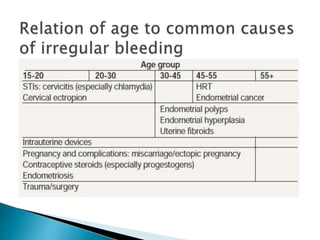
This document discusses normal and abnormal menstrual cycles. It notes that a normal cycle is typically 21-35 days with bleeding for 4-7 days. Abnormal bleeding can include irregular spotting or heavy periods. Menopause and certain medical conditions can also cause irregular cycles. Further evaluation depends on a woman's age, symptoms, medical history and physical exam. Tests like ultrasounds and Pap smears may help identify potential causes like fibroids, infections or cancer. Overall irregular bleeding is common but serious issues are usually rare, so evaluation is tailored based on risk factors.