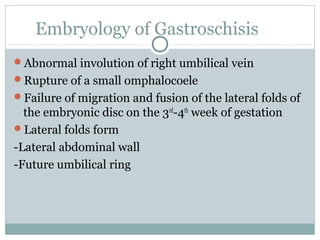
1. The document discusses various abdominal wall defects including omphalocele, gastroschisis, umbilical hernia, prune belly syndrome, bladder extrophy, cloacal exstrophy, and Pentalogy of Cantrell.
2. It describes the embryology, clinical findings, diagnosis, and management of each condition. Common abdominal wall defects like omphalocele and gastroschisis are discussed in detail including their differences.
3. Rare syndromes associated with abdominal wall defects are also mentioned such as Prune Belly Syndrome, Beckwith-Wiedemann Syndrome, and Pentalogy of Cantrell. The document provides an overview of different abdominal wall birth defects.