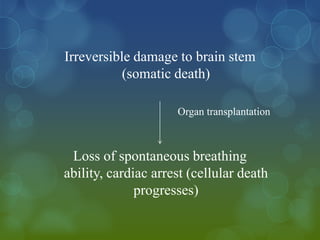
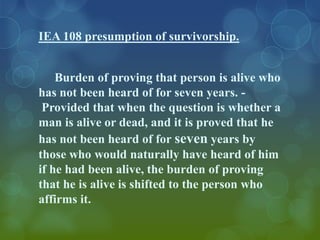
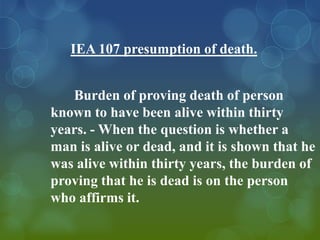
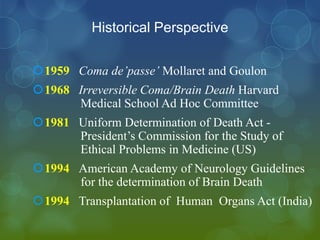
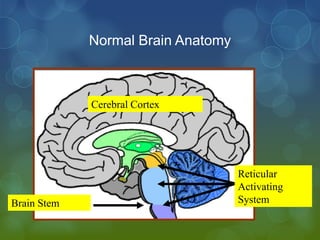
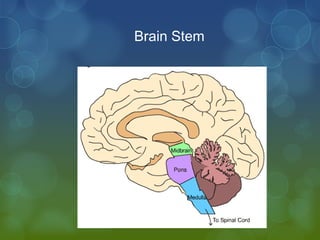
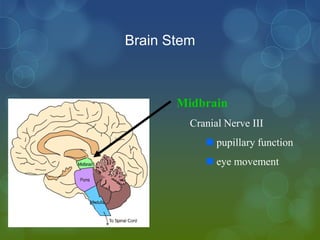
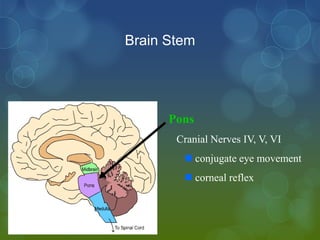
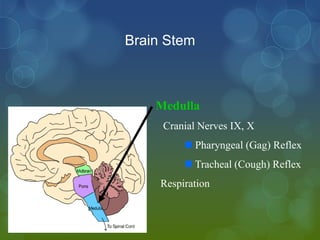
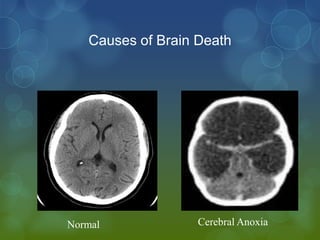
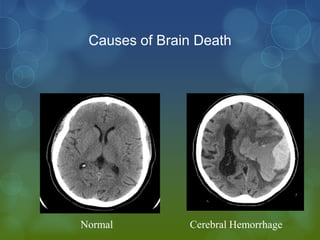
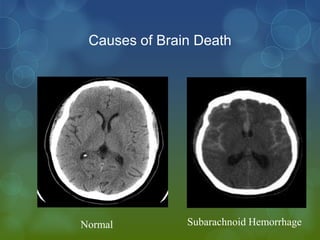
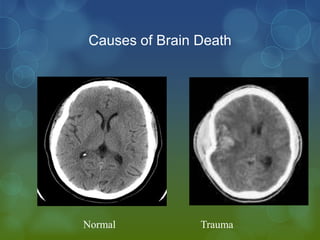
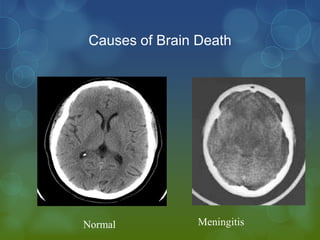
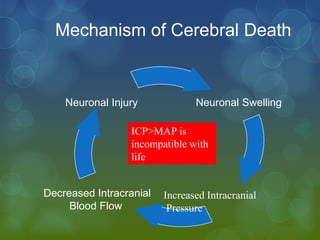
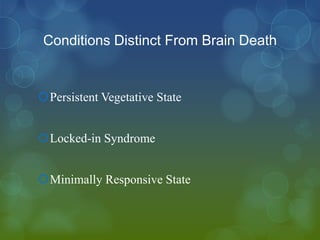
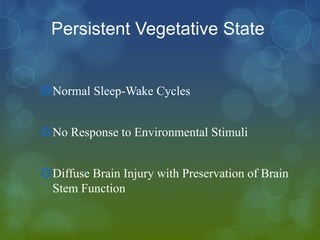
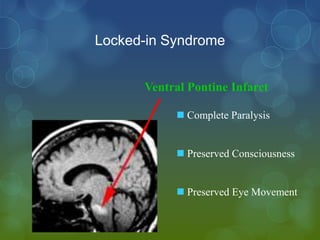
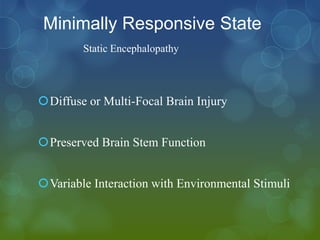
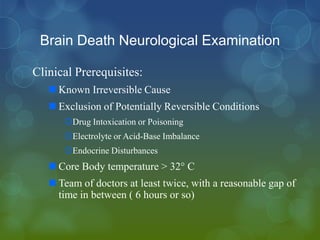
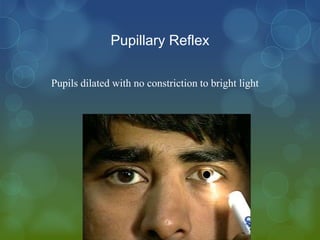
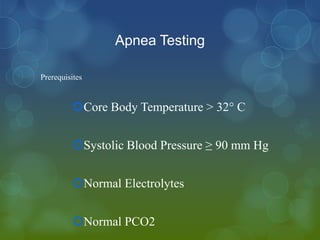
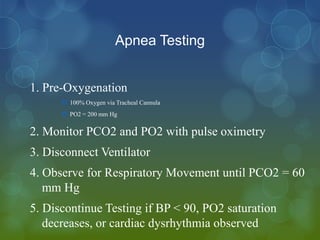
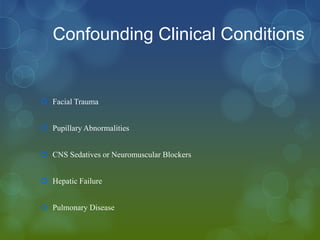
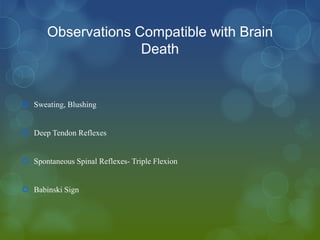
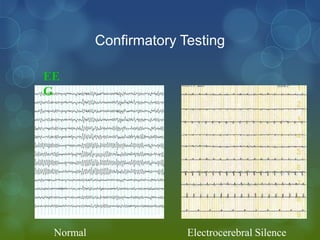
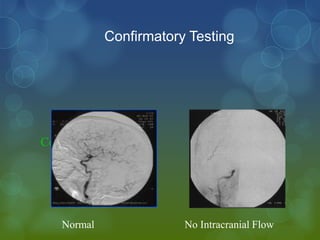
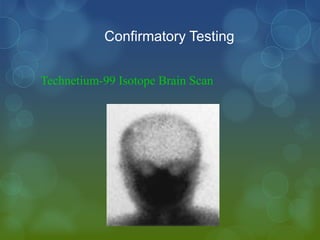
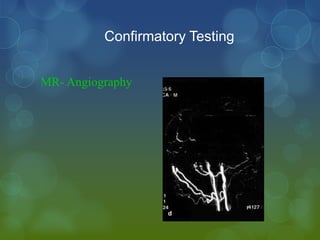
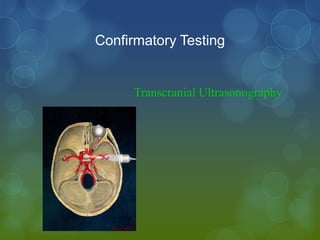
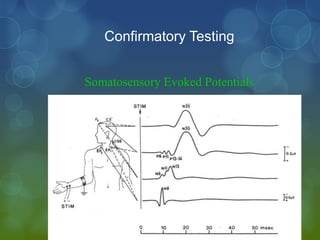
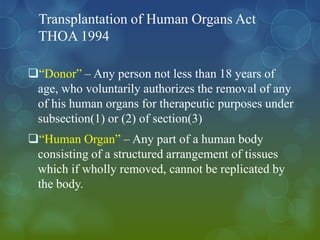
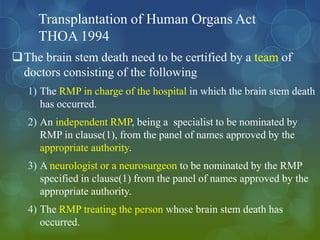
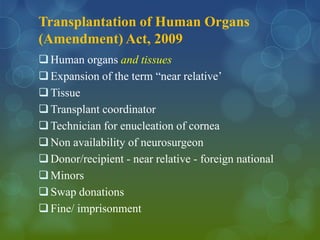
The document summarizes key aspects of death and brain death from a medicolegal perspective. It defines death and outlines the vital systems that cease to function at death. It discusses the presumption of death and survivorship under Indian law. The document then examines the historical definitions of death and milestones in determining brain death. It provides details on the anatomy of the normal brain and causes, mechanisms, and conditions distinct from brain death. The neurological examination for determining brain death and confirmatory testing are described. The key provisions of the Transplantation of Human Organs Act of 1994 and its amendment in 2009 are summarized.