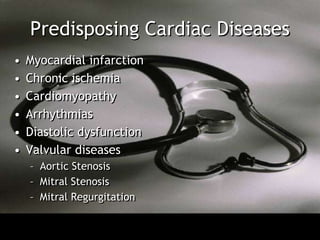
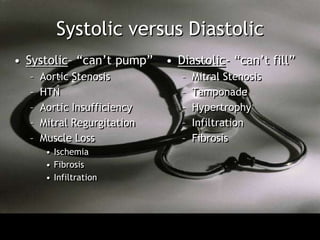
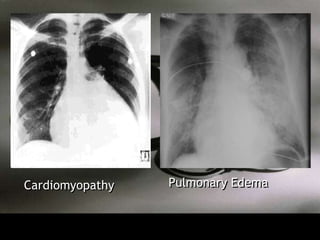
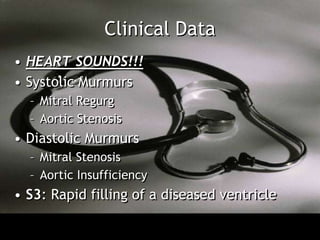
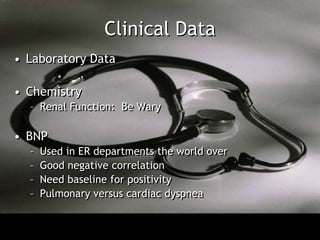
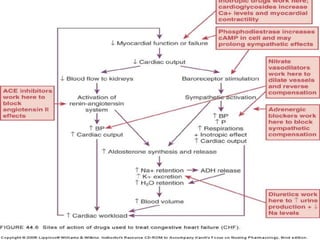
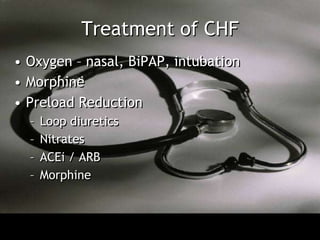
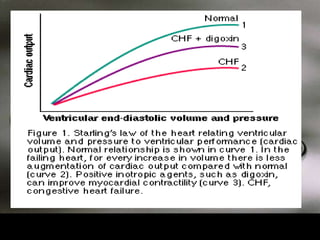
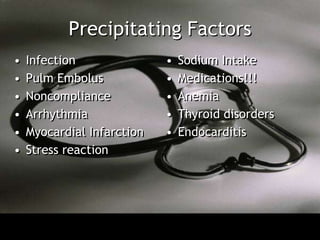
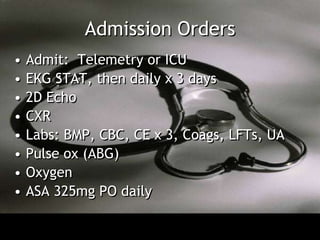
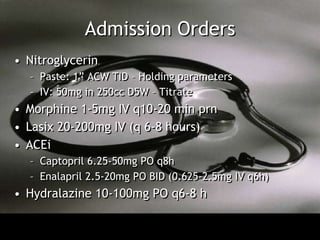
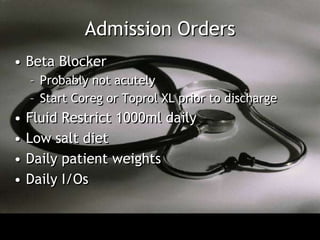
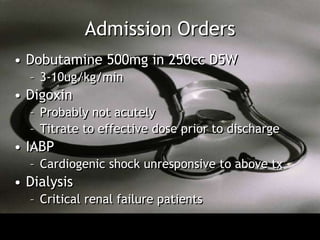
The document discusses congestive heart failure by describing the clinical presentation, underlying cardiac diseases that can cause it, how cardiac physiology relates to concepts like preload, afterload and contractility, classifications of heart failure, clinical exam findings, treatment approaches focusing on reducing preload and afterload and increasing contractility, and sample admission orders for an inpatient with heart failure.