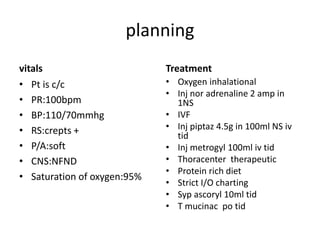
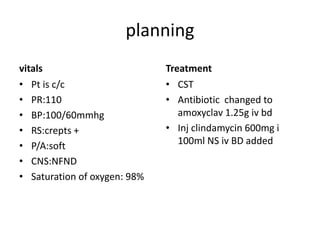
1. A 25-year-old female was admitted with complaints of shortness of breath, loose stools, facial swelling and fever for a week and body pains. Chest X-ray showed consolidation in the right lung. She was diagnosed with pneumonia and pleural effusion, with a relapse of tuberculosis.
2. She was treated with oxygen, antibiotics including piperacillin-tazobactam and metronidazole, thoracentesis, and other supportive care. Her condition improved with treatment.
3. Pneumonia is classified based on location and cause. Risk factors, clinical presentation, diagnosis and management depend on whether it is community-acquired, hospital-acquired, or







![Risk Factors
1. Community-acquired pneumonia.
Risk factors:
a. Alcoholism and smoking; these are associated with a
decreased cough and mucociliary clearance.
b. Age greater than 65 years.
c. Recent viral upper respiratory tract infection; influenza is
classically followed by a bacterial pneumonia caused by S.
pneumoniae or S. aureus.
d. Underlying pulmonary diseases (e.g., chronic obstructive
pulmonary disease [COPD], bronchiectasis, lung cancer).
e. Immunosuppression (e.g., HIV infection, solid organ or stem
cell transplantation, and chronic corticosteroid use).](https://image.slidesharecdn.com/case4pneumonia-220512151812-f0833e4a/85/A-Case-Presentation-on-Pneumonia-15-320.jpg)


















