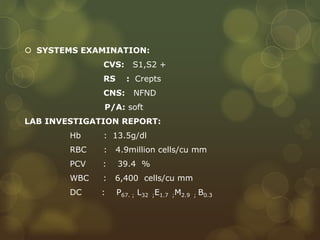
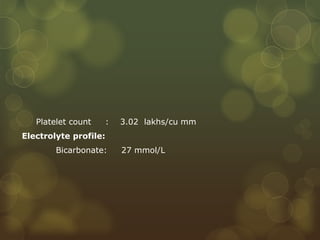
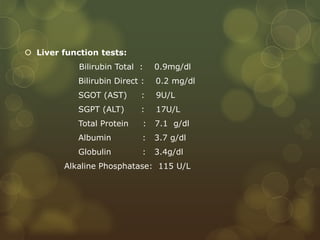
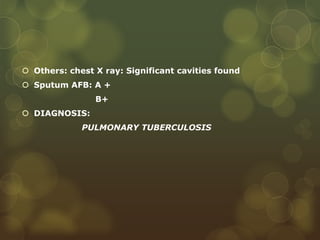
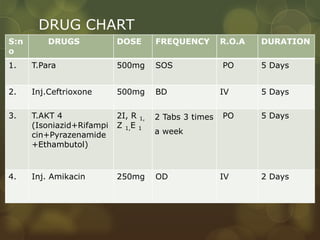
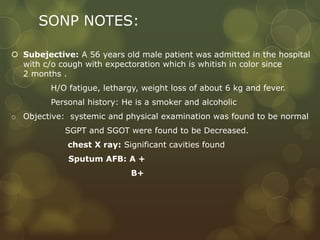
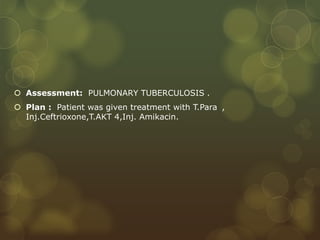
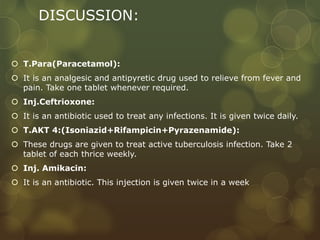
A 56-year-old male patient presented with a 2-month history of cough with whitish sputum, fatigue, weight loss, and fever. Examination found decreased liver enzymes and cavities on chest x-ray. Sputum tests were positive for acid-fast bacilli. He was diagnosed with pulmonary tuberculosis. Treatment included Paracetamol, Ceftriaxone, AKT4 (Isoniazid, Rifampicin, Pyrazinamide, Ethambutol), and Amikacin.