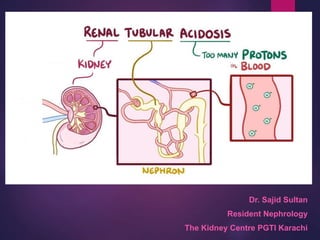
RENAL TUBULAR ACIDOSIS
- 1. Dr. Sajid Sultan Resident Nephrology The Kidney Centre PGTI Karachi
- 2. TUBULAR FUNCTION • 2/3 of glomerular ultra filtrate is reabsorbed from the PT • 60% of Na ia absorbed in the PT & 25% in the ALH &15% in the DT. • All filterd K is reabsorbed in PT & excretion occur in DT and collecting ducts. • H excretion occur in early parts of PT and also DT. • Ca reabsorption occur in parallel with Na reabsorption • Majority of PH is reabsorbed in the PT. • The process of K and H ion excretion and Na reabsorption iall stimulated by aldosteron. • 85% of bicarbonate is reabsorbed in PT and the remaining 15% reabsorbed in the DT
- 4. Acidosis & anion gap < 12 = normal or absence of anion gap RTA carbonic anhydrase inhibitor , Ureterosigmoidostomy pancreatic fistula diarhea
- 5. Acidosis & anion gap >16 =increased anion gap • lactic acidosis • DKA • inborn errors of metabolism • Uremia • poisoning with (salicylate,methanol,ethanol)}
- 6. Normal Urinary Acidification • Urinary acidification involves two processes: • Bicarbonate reabsorption and • Hydrogen ion excretion .
- 7. Normal Urinary Acidification In infants, bicarbonate reabsorption is less efficient, and renal bicarbonate excretion may occur at serum concentrations less than 22 mmol/L. The hydrogen ion in the tubular lumen binds with bicarbonate and, under the influence of carbonic anhydrase, is converted to carbon dioxide and water.
- 8. Normal Urinary Acidification Secretion of the daily acid load (approximately 1 mEq/kg/24 hr produced during normal cellular processes) is accomplished by hydrogen ion secretion Approximately 85% of the filtered bicarbonate is reabsorbed in the proximal tubule . The remaining 15% of bicarbonate is reabsorbed distally
- 9. DEFINITION • metabolic acidosis due to a defect at the level of the renal tubule. • non-anion gap or hyperchloremic metabolic acidosis ------------ from loss of bicarbonate inability to reabsorb HCO3 or retention of hydrogen ion (inability to excrete).
- 10. 2----1-----4 proximal 2, distal 1, collecting tubules 4
- 12. Find the ODD for caphstones
- 13. Odd is one and its different
- 14. The odd one has the stones as well
- 15. TYPES OF RTAs • Distal ------------------loss of hydrogen ion secretion into urine • Proximal ---------------- loss of bicarbonate reabsorption • Hypoaldosteronism or hyperkalemic (Type IV): ----------- distal tubule resistance to aldosterone ----------loss of potassium excretion--------hyperkalemia ------------ suppression of ammonia excretion.
- 17. Proximal (Type II) Renal Tubular Acidosis • Pathogenesis Impaired proximal tubule bicarbonate reabsorption. Isolated forms of inherited or acquired proximal occur, Autosomal dominant forms, As well as an autosomal recessive form associated with ocular abnormalities, have been reported. More typically, proximal rta occurs as a component of global proximal tubule dysfunction or fanconi syndrome. Both autosomal dominant and autosomal recessive forms of primary fanconi syndrome occur. In addition, secondary fanconi syndrome may occur as a component of one of several inherited renal tubular disorders or in acquired disease states.
- 18. Pathogenesis
- 19. Pathogenesis
- 21. Clinical Manifestations • Patients with isolated, sporadic, or inherited proximal RTA commonly present with growth failure in the first year of life. • Additional symptoms may include polyuria, dehydration (due to sodium losses), anorexia, vomiting, constipation, and hypotonia.
- 22. Clinical Manifestations Patients with PRIMARY FANCONI SYNDROME will have additional symptoms secondary to phosphate wasting such as rickets. Those with systemic diseases will present with additional signs and symptoms specific to their underlying disease. A non-anion gap metabolic acidosis will be present. Urinalysis in patients with isolated proximal RTA is generally unremarkable. The urine pH is acidic (<5.5), because distal acidification mechanisms are intact in these patients.
- 23. Distal (Type I) Renal Tubular Acidosis Pathogenesis Impaired distal urinary acidification (hydrogen ion secretion). Damaged or impaired functioning of one or more transporters or proteins involved in the acidification process, including the h+/atpase, the hco3-/cl- anion exchangers or the components of the aldosterone pathway. Because of impaired hydrogen ion excretion, urine ph cannot be reduced below 5.5, despite the presence of severe metabolic acidosis. Loss of sodium bicarbonate results in hyperchloremia and hypokalemia.
- 24. Pathogenesis Hypercalciuria is usually present and may lead to nephrocalcinosis or nephrolithiasis. Chronic metabolic acidosis also impairs urinary citrate excretion. Hypocitraturia further increases the risk of calcium deposition in the tubules. Bone disease is common, resulting from mobilization of organic components from bone to serve as buffers to chronic acidosis. Both primary sporadic or inherited forms occur. As with proximal RTA, distal RTA can also occur as a complication of either inherited or acquired diseases of the distal tubules.
- 25. Toluene induced RTA 1 Present in glue Inhibits proton secretion Produceshipuuirc and benxzopic acid Buffered by bicarbonate, resulting in acidosis.
- 27. Clinical Manifestations Non-anion gap metabolic acidosis and growth failure. However, distinguishing features of distal RTA include nephrocalcinosis and hypercalciuria. The phosphate and massive bicarbonate wasting characteristic of proximal RTA is generally absent.
- 28. Hyperkalemic (Type IV) Renal Tubular Acidosis • Pathogenesis: impaired aldosterone production (hypoaldosteronism) OR impaired renal responsiveness to aldosterone ("pseudo" hypoaldosteronism). Because aldosterone has a direct effect on the H+ ATPase responsible for hydrogen secretion, acidosis results. In addition, aldosterone is a potent stimulant for potassium secretion in the collecting tubule. Loss of aldosterone effect results in hyperkalemia.
- 29. Pathogenesis: This further affects acid-base status by inhibiting ammoniagenesis and, thus, hydrogen ion excretion. Aldosterone deficiency typically occurs as a result of adrenal gland disorders such as Addison disease or congenital adrenal hyperplasia (CAH).
- 30. Pathogenesis: In children, aldosterone unresponsiveness is a more common cause of type IV RTA. This may occur transiently, during an episode of acute pyelonephritis or acute urinary obstruction, or chronically, particularly in infants and children with a history of obstructive uropathy. The latter patients may have significant hyperkalemia, even in instances when renal function is normal or only mildly impaired. Rare examples of inherited forms of type IV RTA have been identified.
- 32. Clinical Manifestations. Patients with type IV RTA, like those with types I and II RTA, may present with growth failure in the first few years of life. Polyuria and dehydration (from salt wasting) are common. Rarely, patients (especially those with pseudohypoaldosteronism type 1) will present with life- threatening hyperkalemia.
- 33. Clinical Manifestations. Patients with obstructive uropathies may present acutely with signs and symptoms of pyelonephritis, such as fever, vomiting, and foul-smelling urine. Laboratory tests reveal a hyperkalemic non-anion gap metabolic acidosis. Urine may be alkaline or acidic. Elevated urine sodium levels with inappropriately low urine potassium levels reflect the absence of aldosterone effect.
- 34. Diagnosis of RTA • confirm the presence of and nature of the metabolic acidosis. • assess renal function. • rule out other causes of metabolic acidosis, such as diarrhea ( which is extremely common) . • identify electrolyte abnormalities (K,Na,Cl) • blood urea nitrogen, calcium, phosphorus, and creatinine and pH blood should be obtained by venous puncture. Traumatic blood draws (such as heel stick specimens) or prolonged specimen transport time can lead to falsely low bicarbonate levels, often in association with an elevated serum potassium value.
- 35. Diagnosis of RTA True hyperkalemic acidosis is consistent with type IV RTA, whereas the finding of normal or low potassium suggests type I or II.
- 36. Urine pH Urine pH may help distinguish distal from proximal causes. A urine pH of less than 5.5in the presence of acidosis suggests proximal RTA, whereas patients with distal RTA typically have a urine pH of more than 5.5
- 39. URINALYSIS A urinalysis should also be obtained to determine the presence of glycosuria, proteinuria, or hematuria suggesting the possibility of more global tubular damage or dysfunction .
- 42. Urine Calcium Random or 24-hr urine calcium and creatinine measurements will identify hypercalciuria .
- 43. Renal ultrasound A renal ultrasound should be obtained to identify underlying structural abnormalities such as obstructive uropathies as well as to determine the presence of nephrocalcinosis.
- 44. Ultrasound examination of a child with distal renal tubular acidosis demonstrating medullary nephrocalcinosis
- 45. Treatment: • Patients with proximal RTA often require large quantities of bicarbonate, up to 20 mEq/kg/24 hr in the form of sodium bicarbonate or sodium citrate solution (Bicitra or Shohl's solution). Also we have( polycitra solution) which same as bictra with adding of potassium citrate. • The base requirement for distal RTAs is generally in the range of 2-4 mEq/kg/24 hr, although patient requirements may vary . • Patients with distal RTA should be monitored for the development of hypercalciuria. Those with symptomatic hypercalciuria (e.g., recurrent episodes of gross hematuria), nephrocalcinosis, or nephrolithiasis may require thiazide diuretics to decrease urine calcium excretion.
- 46. Treatment of RTA cont. • Patients with type IV RTA may require chronic treatment for hyperkalemia with sodium-potassium exchange resin (Kayexalate). • The mainstay of therapy in all forms of RTA is bicarbonate replacement .
- 47. Save the bones: Rickets may be present in primary renal tubular acidosis (RTA), particularly in type II or proximal RTA. Administration of sufficient bicarbonate to reverse acidosis stops bone dissolution and the hypercalciuria that is common in distal RTA. Proximal RTA is treated with both bicarbonate and oral phosphate supplements to heal bone disease. Doses of phosphate similar to those used in familial hypophosphatemia or Fanconi syndrome should be used. Vitamin D is needed to offset the secondary hyperparathyroidism that complicates oral phosphate therapy
- 48. Thanks……
