The document provides a comprehensive overview of central nervous system infections, including types of meningitis (bacterial, viral, fungal, parasitic) and their common etiological agents, highlighting the significance of certain pathogens based on patient age and predisposition. It details the clinical features, diagnostic approaches, and treatment options for various forms of meningitis, including pneumococcal and meningococcal meningitis, as well as neonatal cases and viral encephalitis. Additionally, the document discusses preventative measures such as vaccination and the implications of emerging antibiotic resistance.




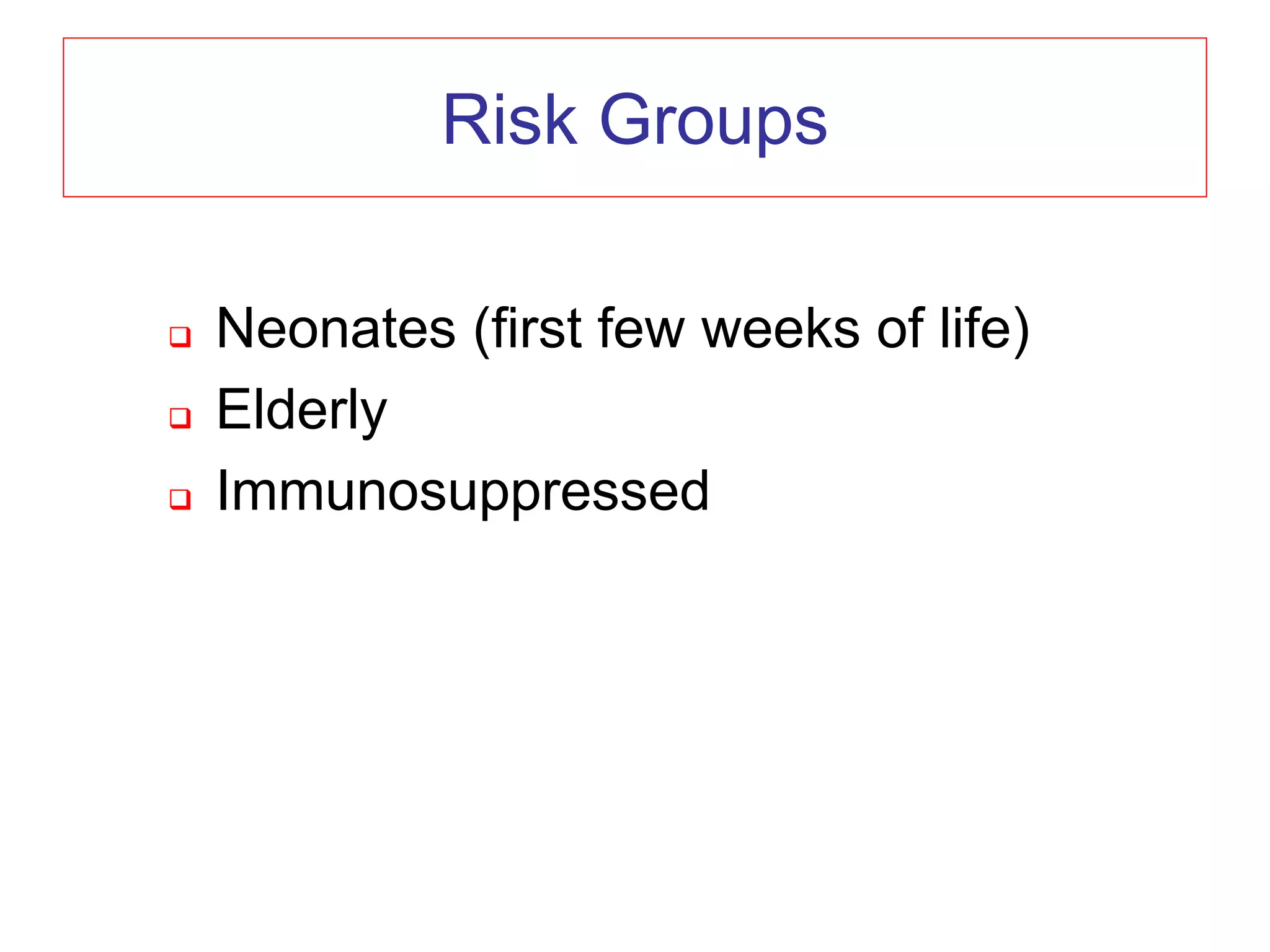



















































































![EMPIRIC THERAPY OF MENINGITIS IN THE
ADULT
Clinical Setting Likely Pathogens Therapy
Community-acquired S. pneumoniae Ceftriaxone
N. meningitidis 2 gm q12h
[Listeria] +
[H. influenzae] Ampicillin 2 gm q4h
Closed head trauma S. pneumoniae Pen G 3-4 mu q4h
Streptococci +
Vancomycin 1-2 gm q12h](https://image.slidesharecdn.com/5-acns-230215091523-289e886c/75/5-a-CNS-pptx-90-2048.jpg)
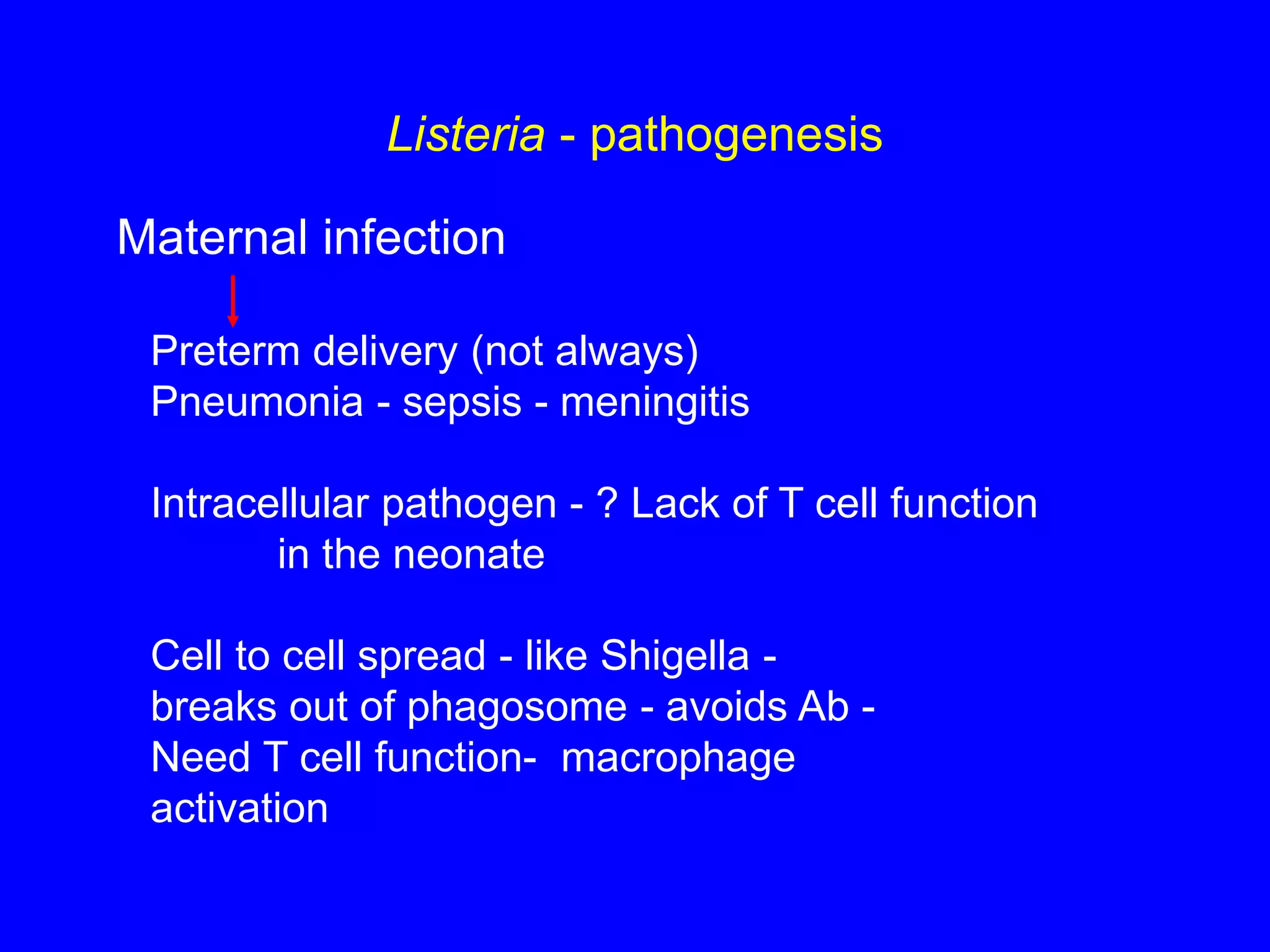
![EMPIRIC THERAPY OF MENINGITIS IN THE
ADULT
Clinical Setting Likely Pathogens Therapy
High risk patients S. aureus Vancomycin 2-3 gm/d
Compromised hosts Gram negative +
Neurosurgical bacilli Ceftazidime 2 gm q8h or
Open head injury Listeria Cefepime 2 gm q8h
Nosocomial [Ceftriaxone 2 gm q12h]
Elderly [Cefotaxime 2 gm q4h]
+/-
Ampicillin 2 gm q4h](https://image.slidesharecdn.com/5-acns-230215091523-289e886c/75/5-a-CNS-pptx-91-2048.jpg)

