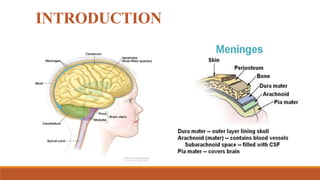
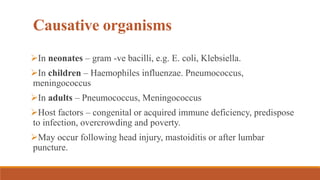
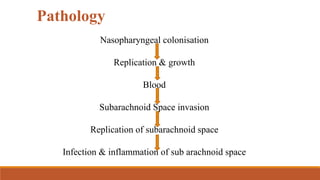
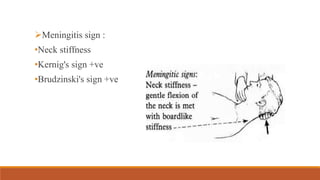
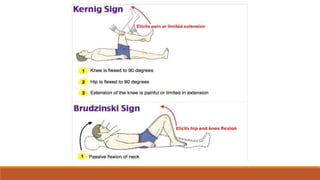
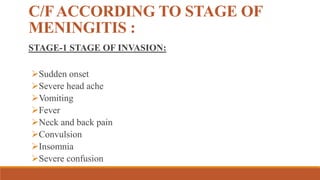
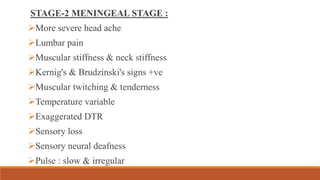
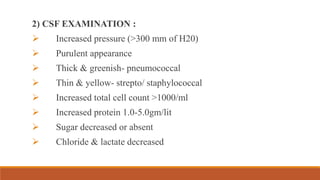
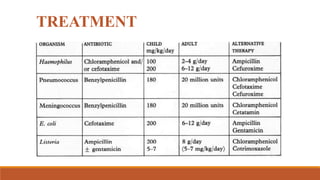
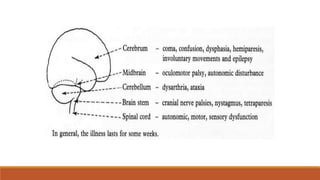
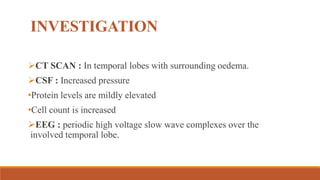
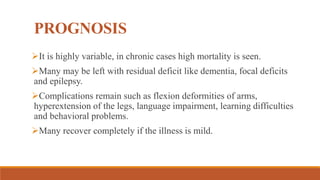
This document discusses meningitis and encephalitis. It defines meningitis as an infection of the meninges and encephalitis as an inflammation of the brain parenchyma. It outlines the different types of meningitis and common causative organisms. It describes the clinical features, investigations, complications, prognosis and treatment for both conditions. The goals of physical therapy for patients with these inflammatory central nervous system disorders are also mentioned.