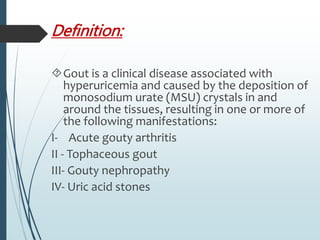
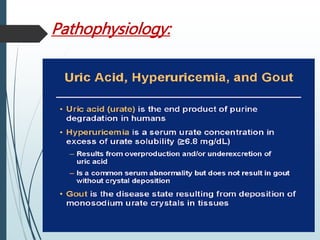
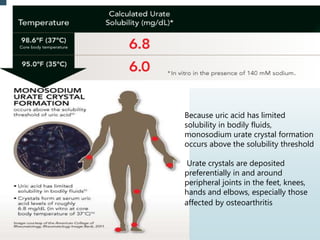
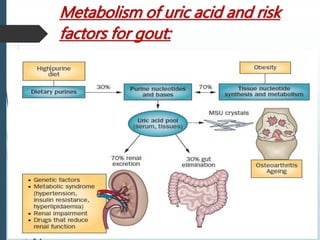
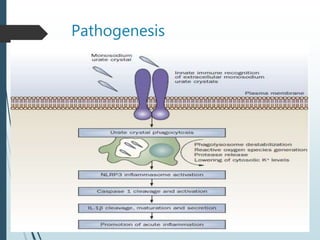
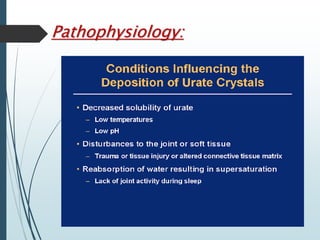
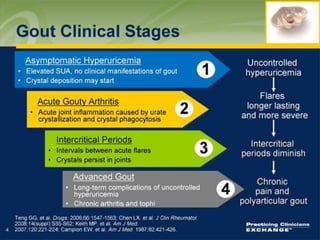
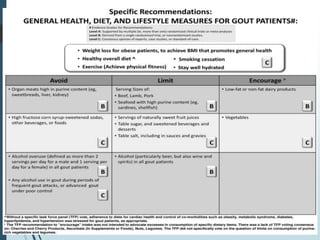
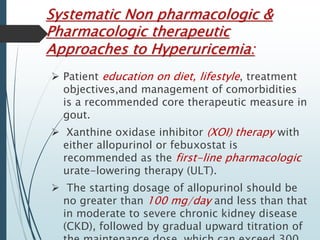
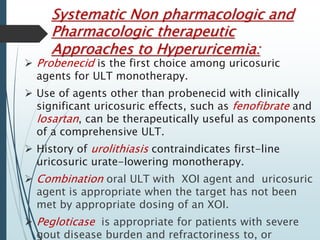
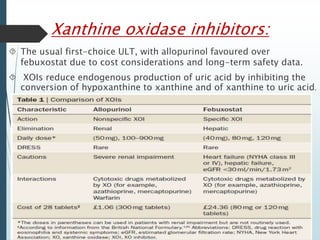
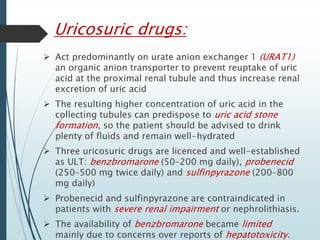
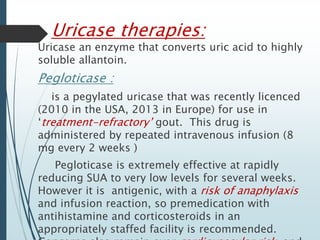
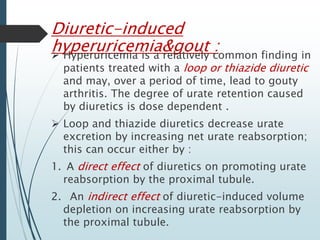
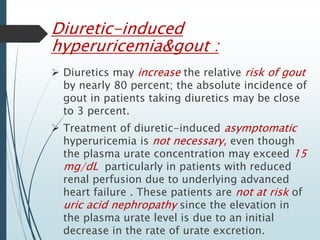
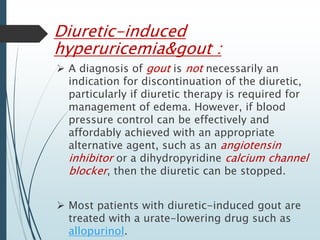
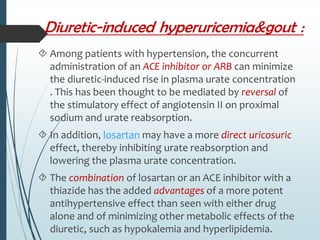
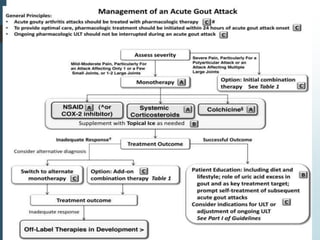
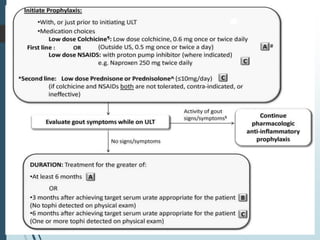
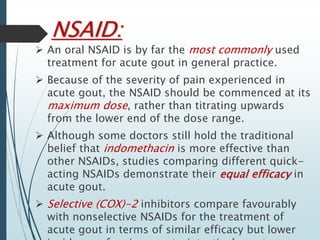
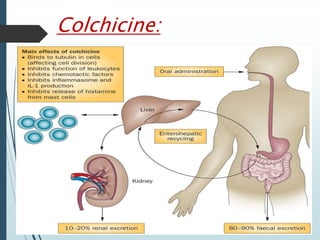
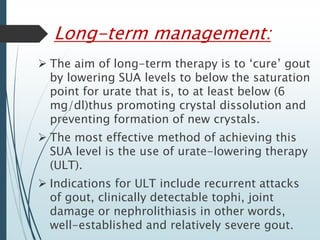
Gout is a clinical disease caused by the deposition of monosodium urate crystals in tissues, which can cause acute gouty arthritis, tophaceous gout, gouty nephropathy, or uric acid stones. The aims of gout treatment are to improve outcomes by suppressing flares, eliminating gout permanently, resolving tophi, and managing comorbidities. First-line treatment for hyperuricemia involves xanthine oxidase inhibitors or uricosuric agents to lower uric acid levels. Diuretics can cause hyperuricemia and gout by increasing urate reabsorption, and treatment may involve changing medications or adding allopurinol.