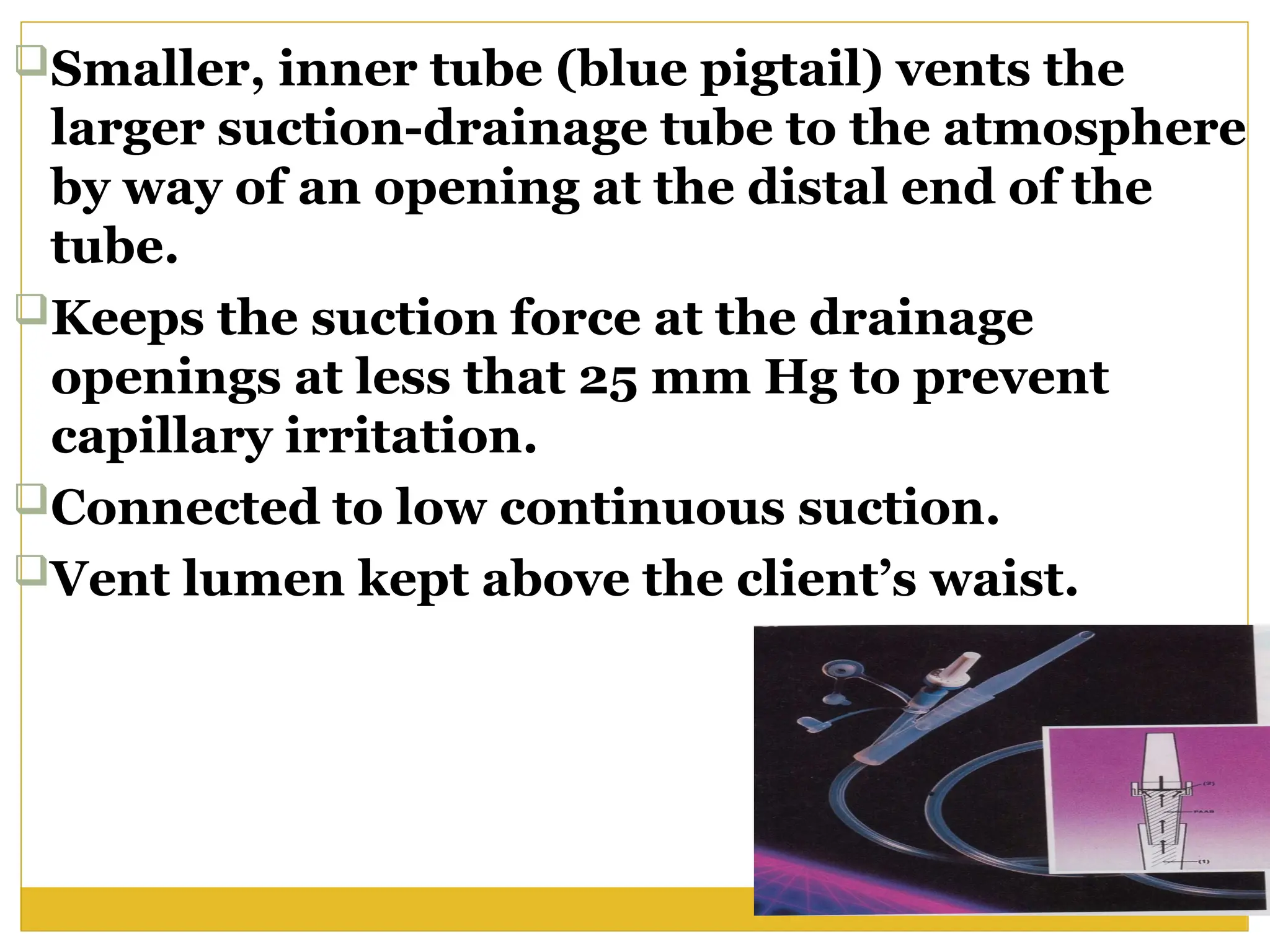
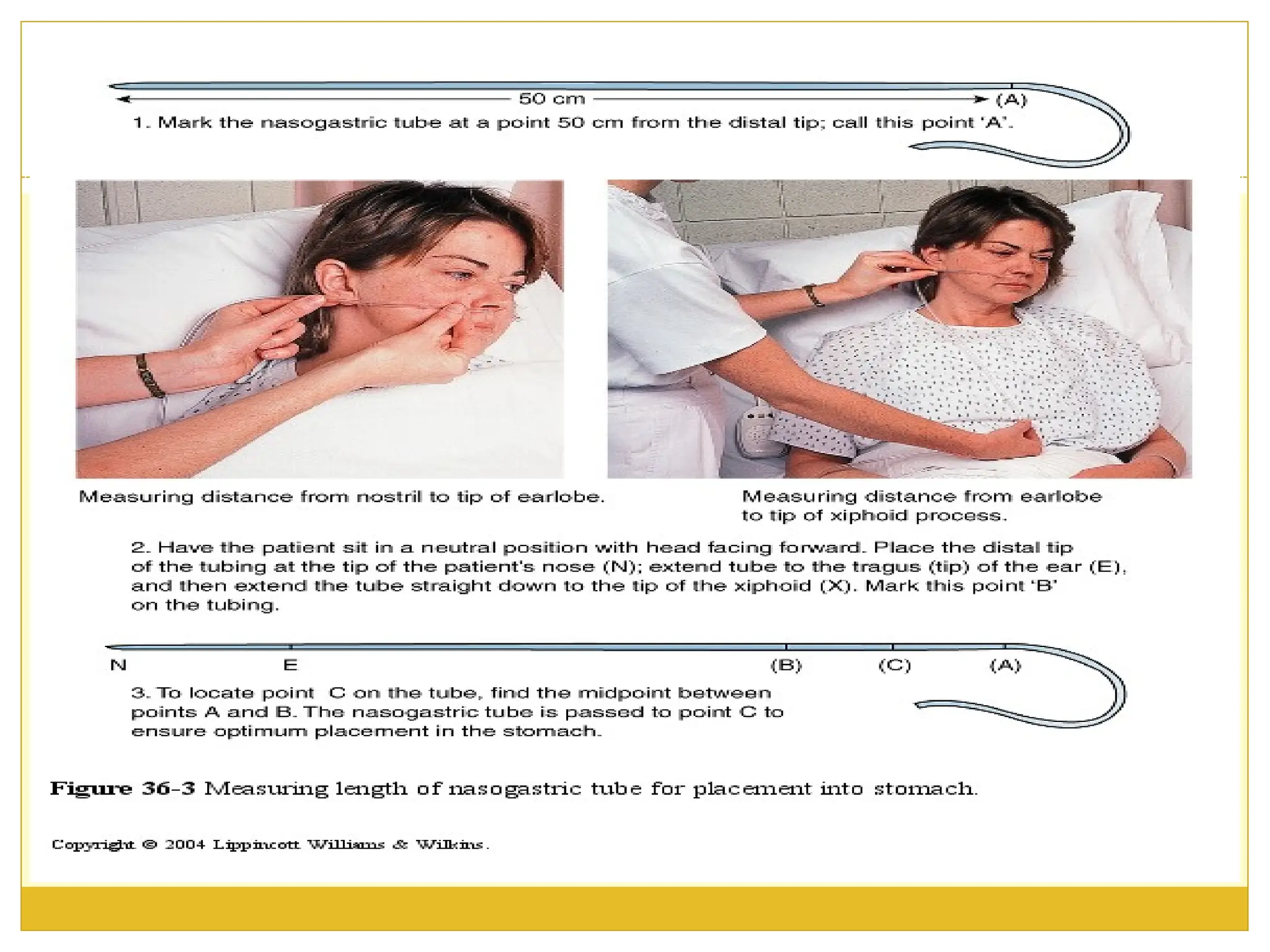
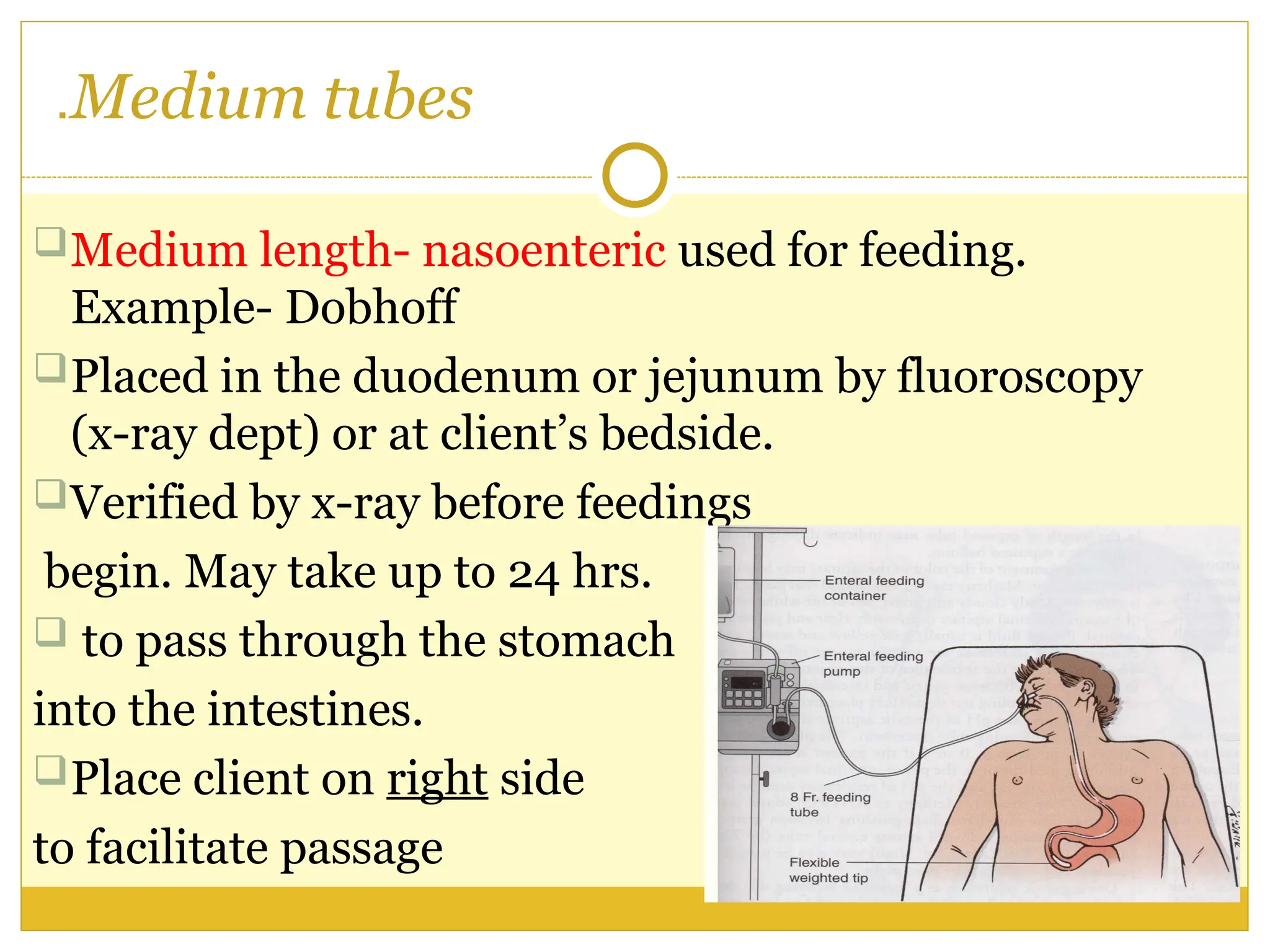
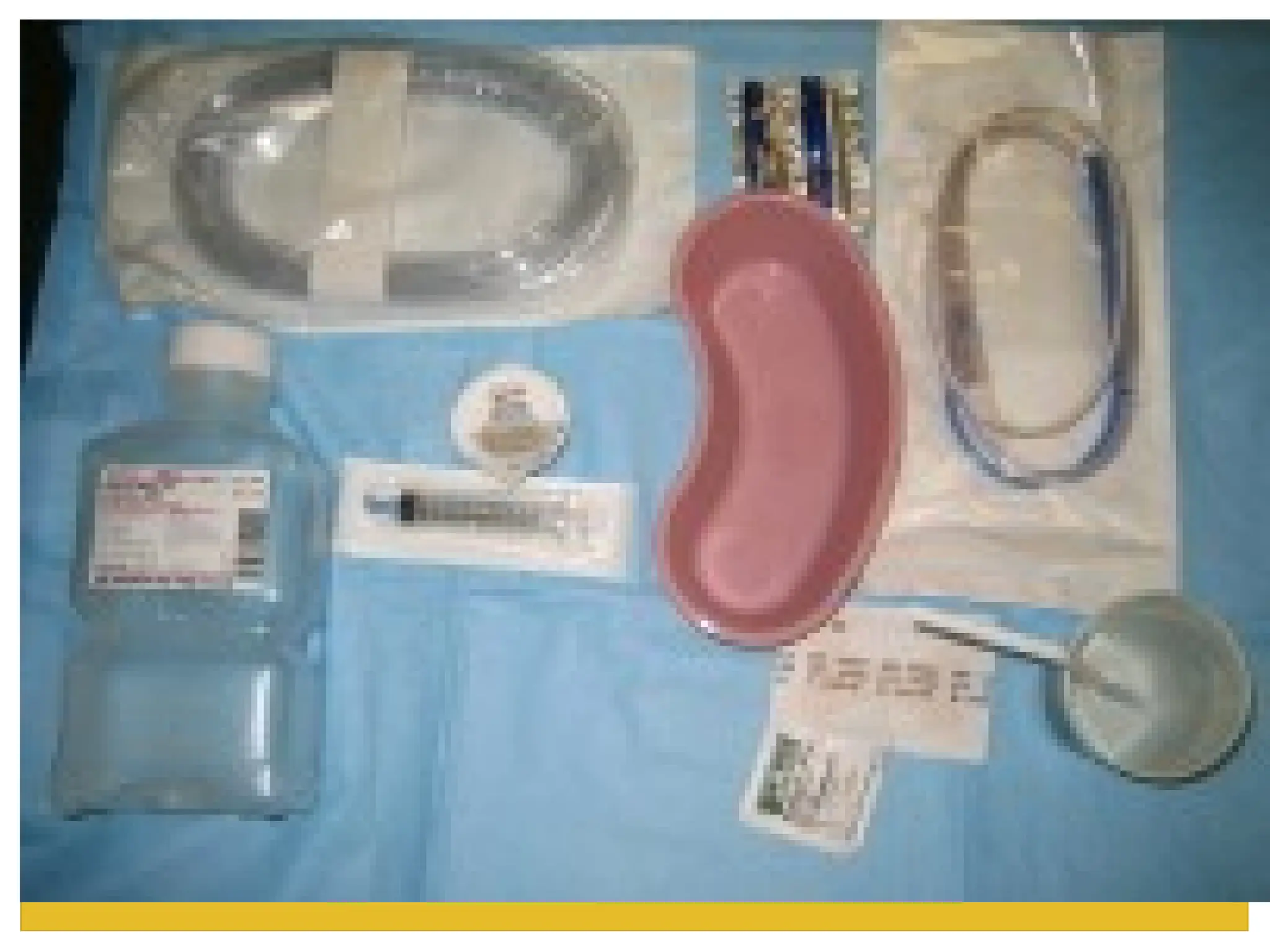
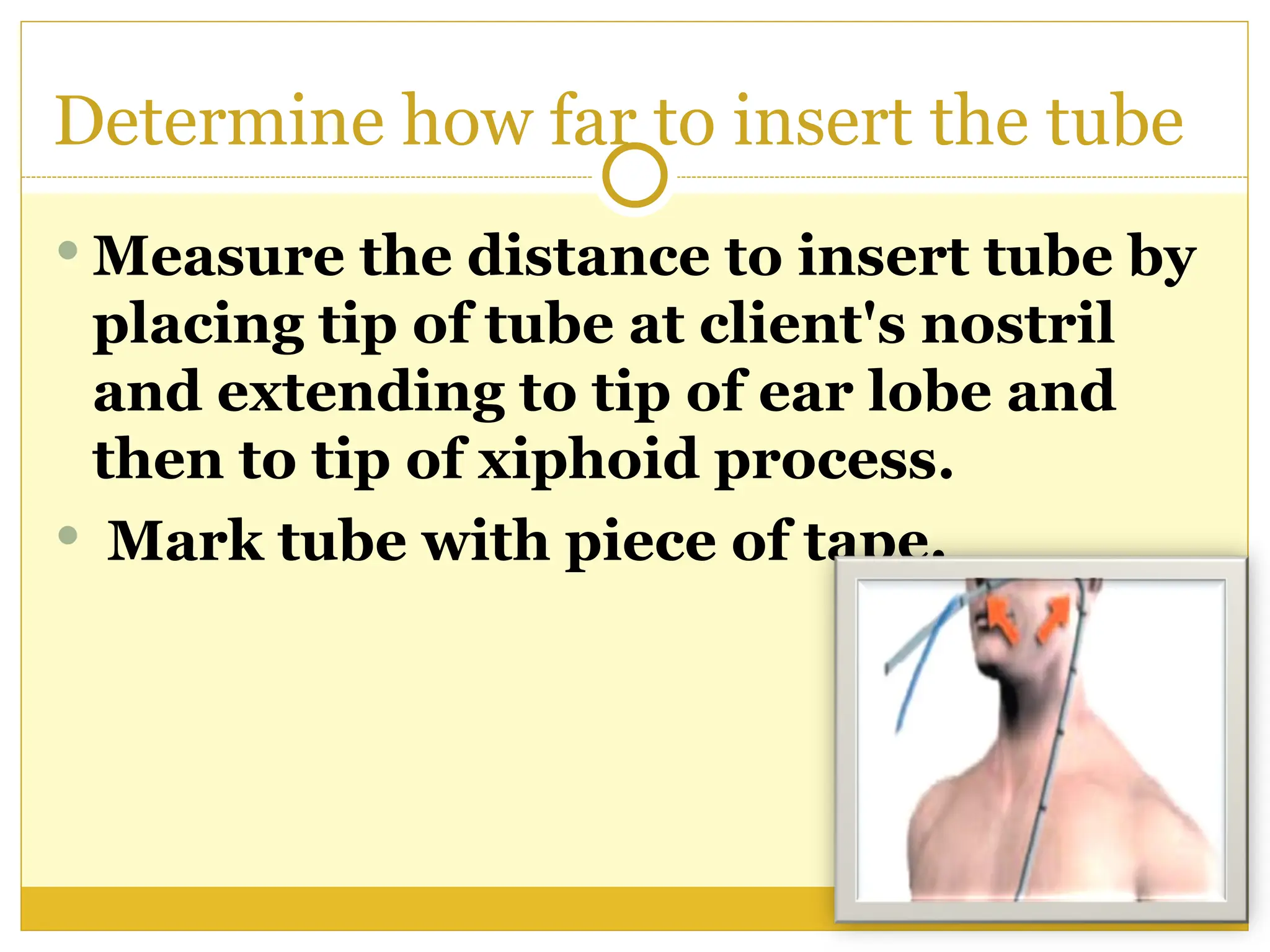
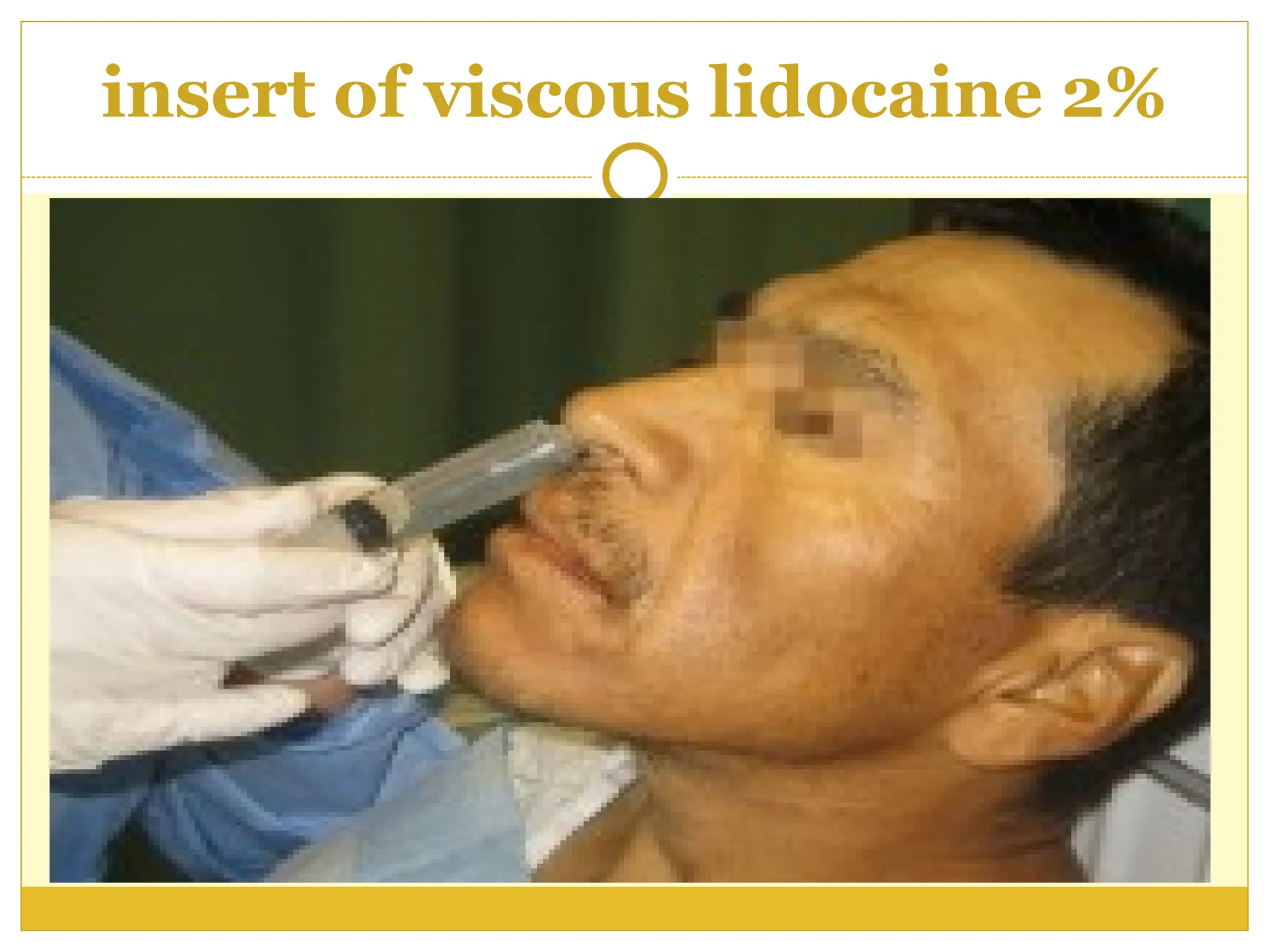
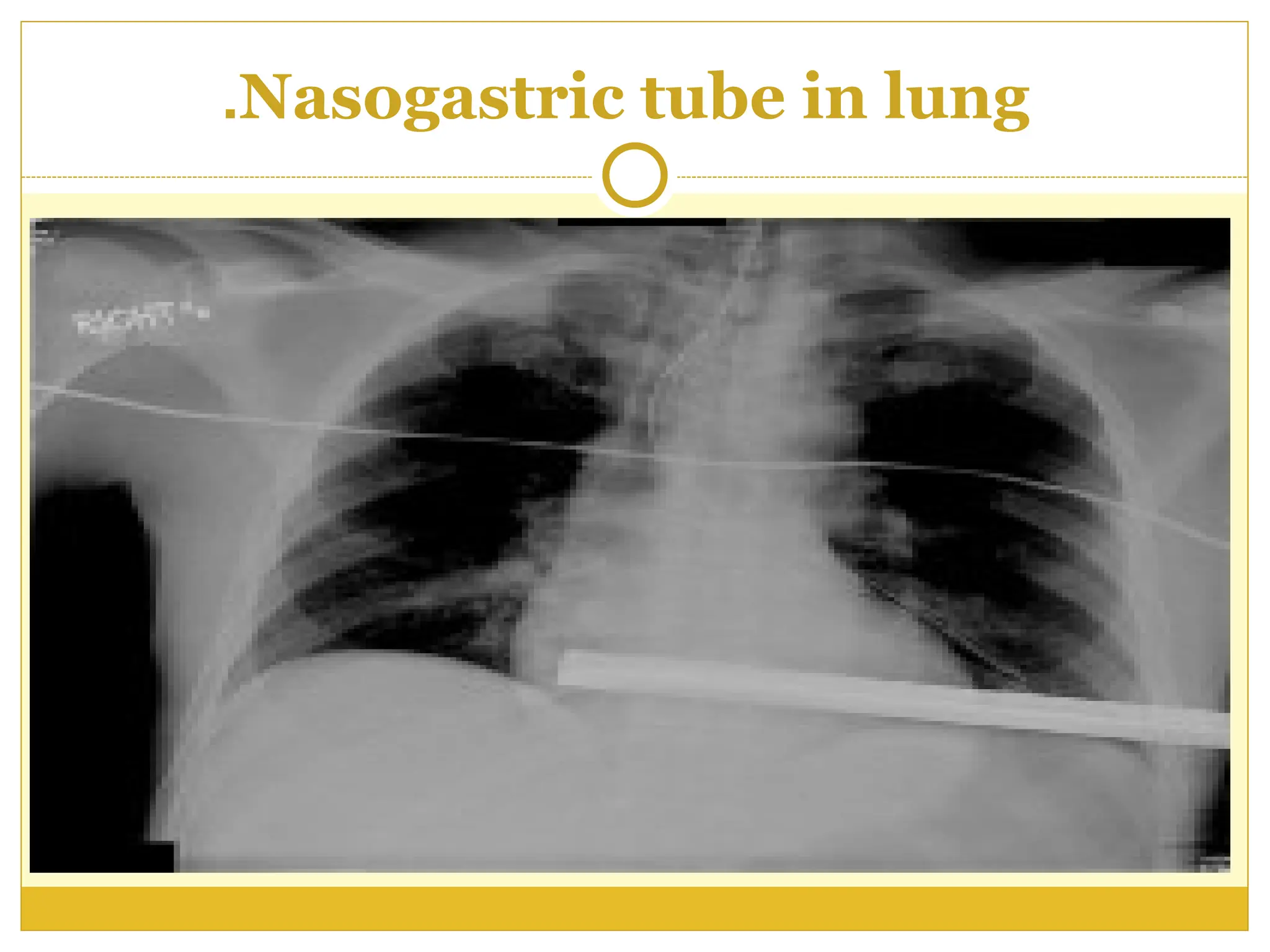
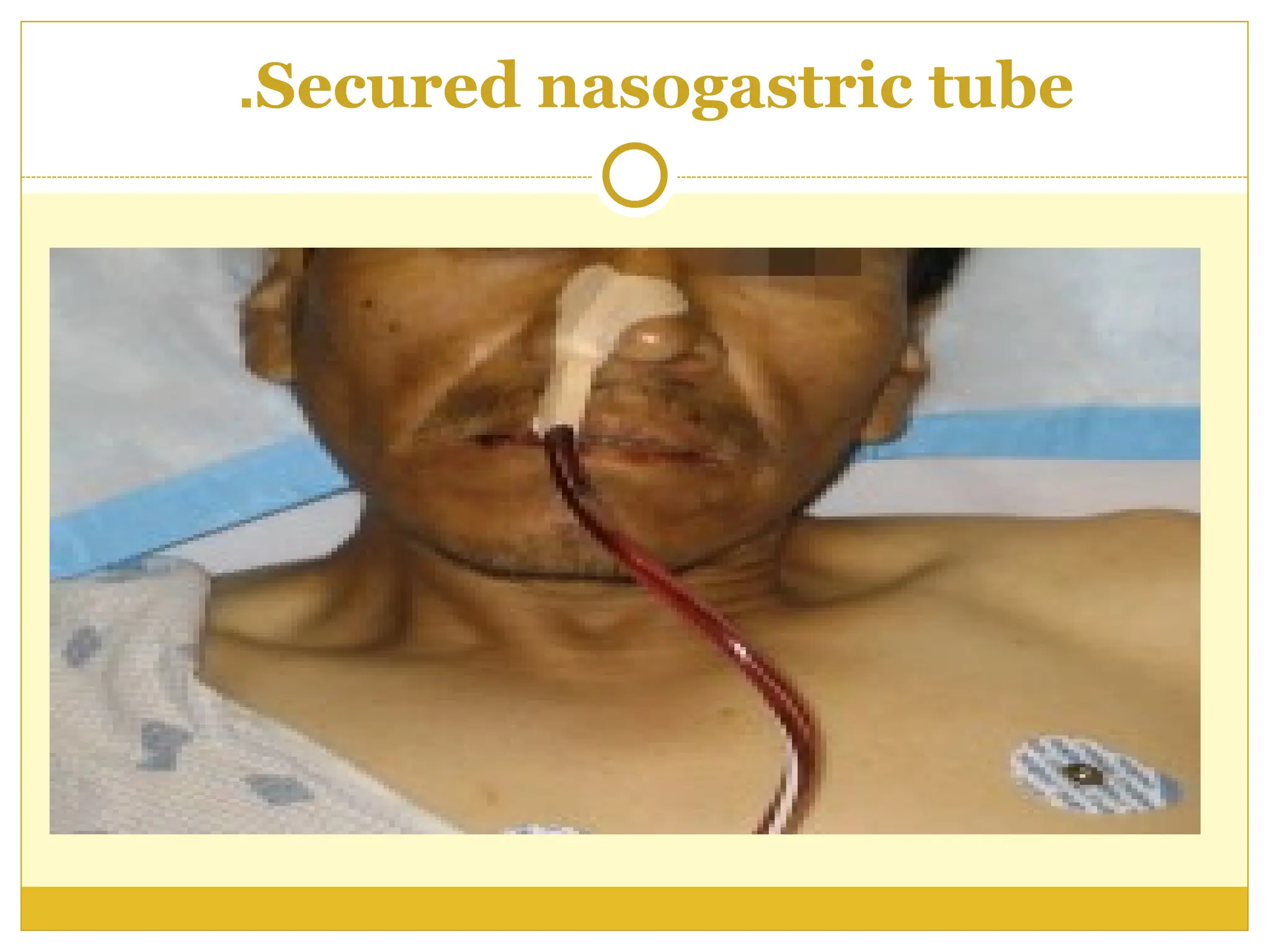
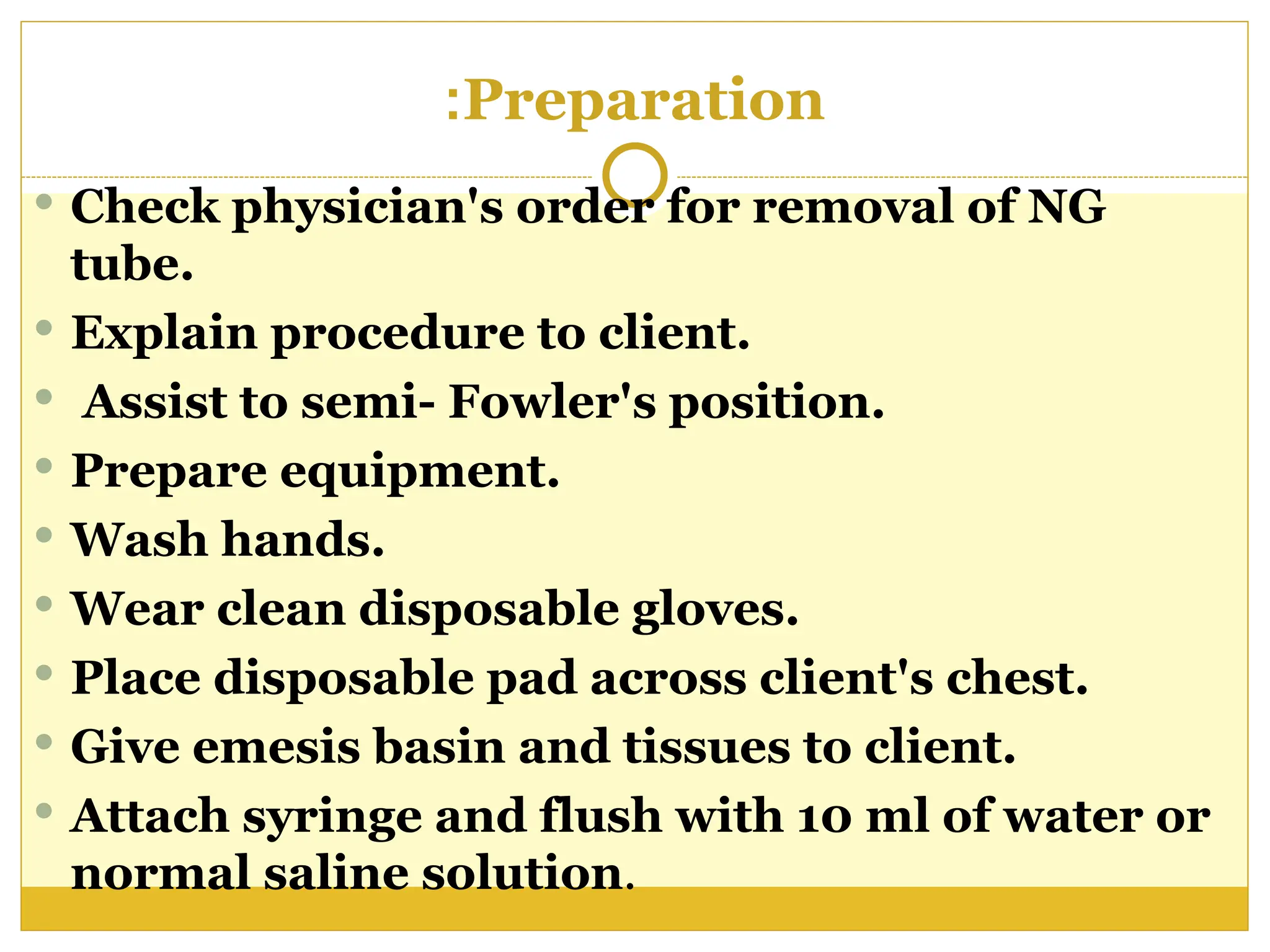
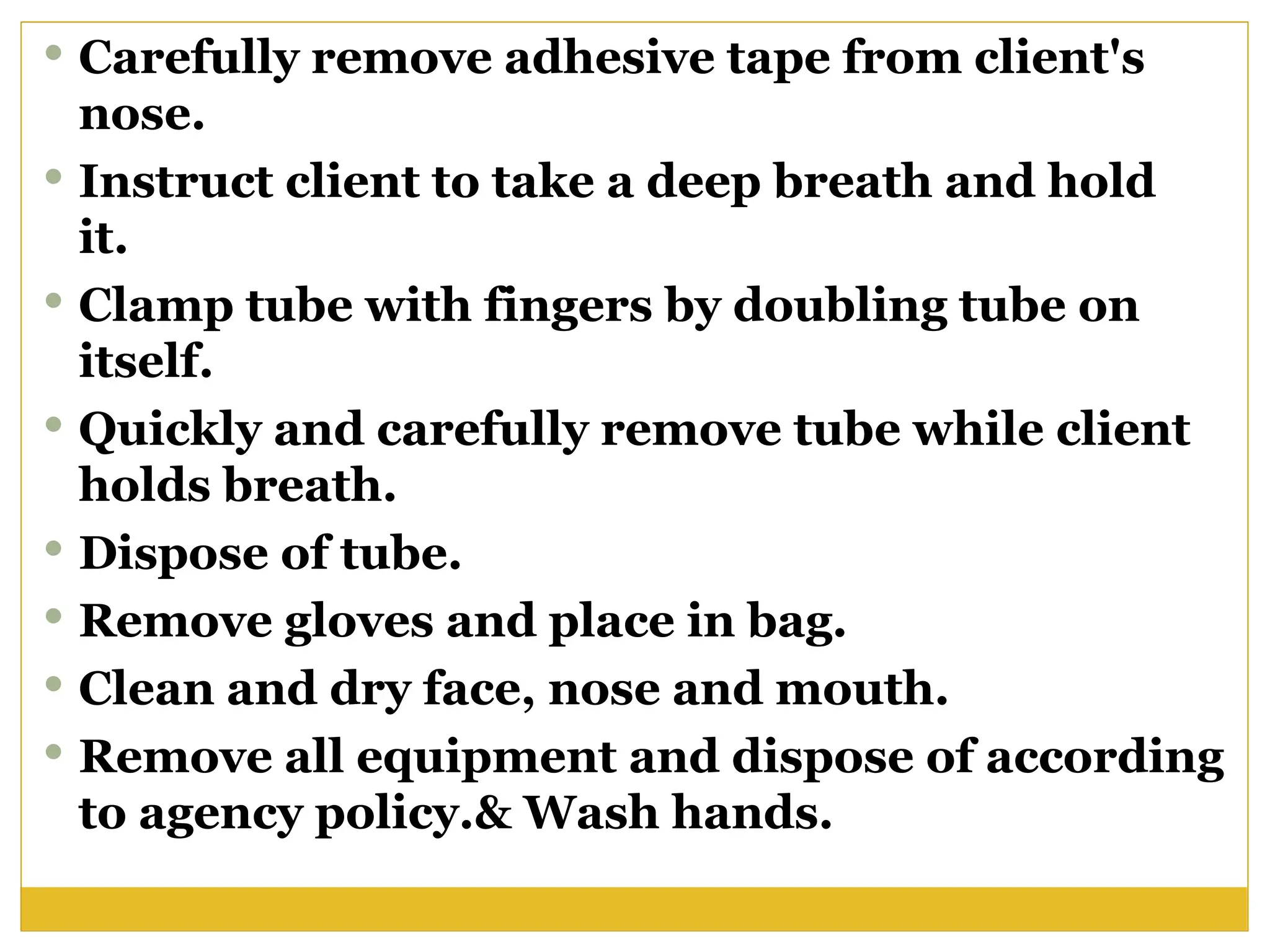
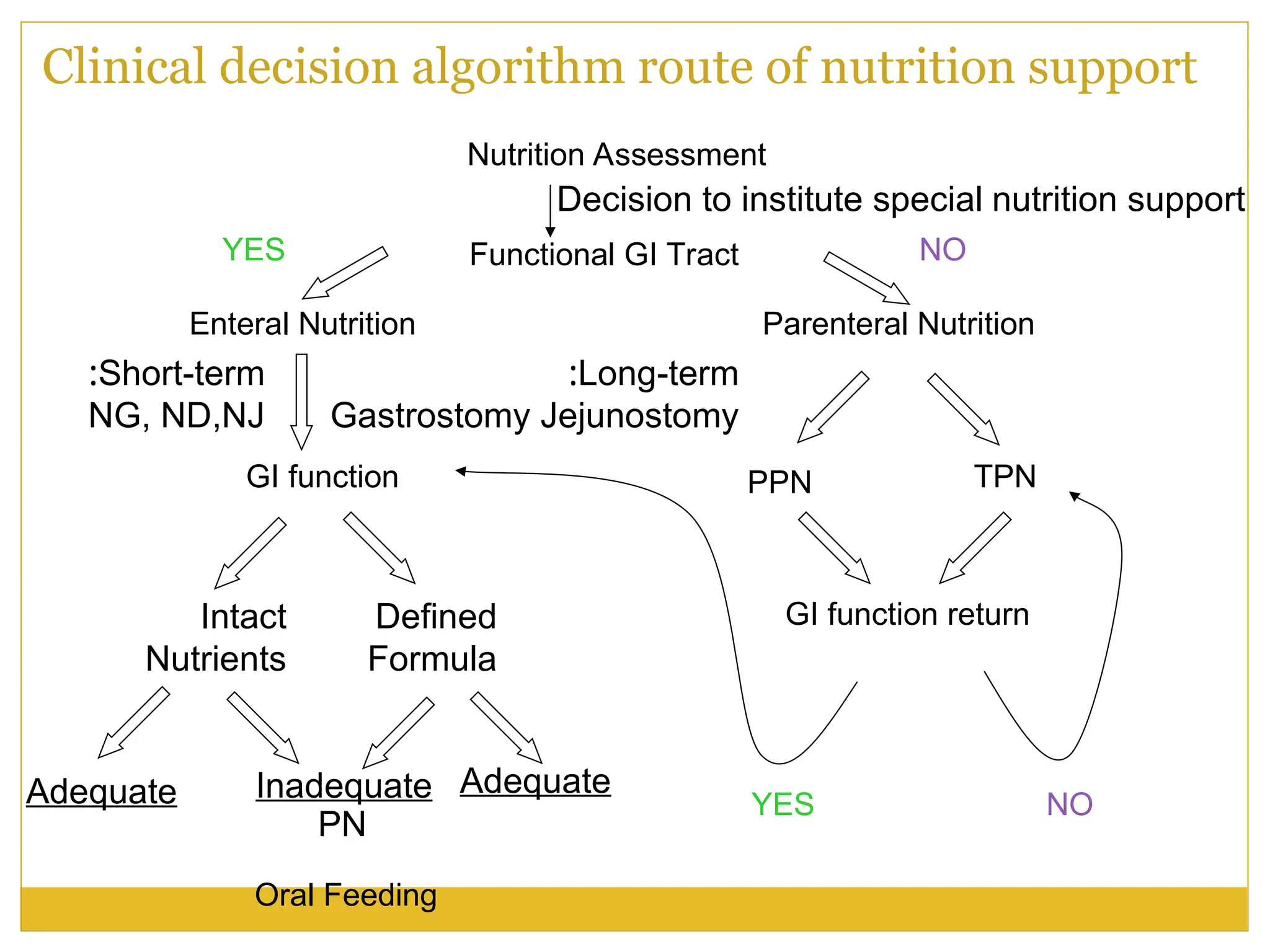
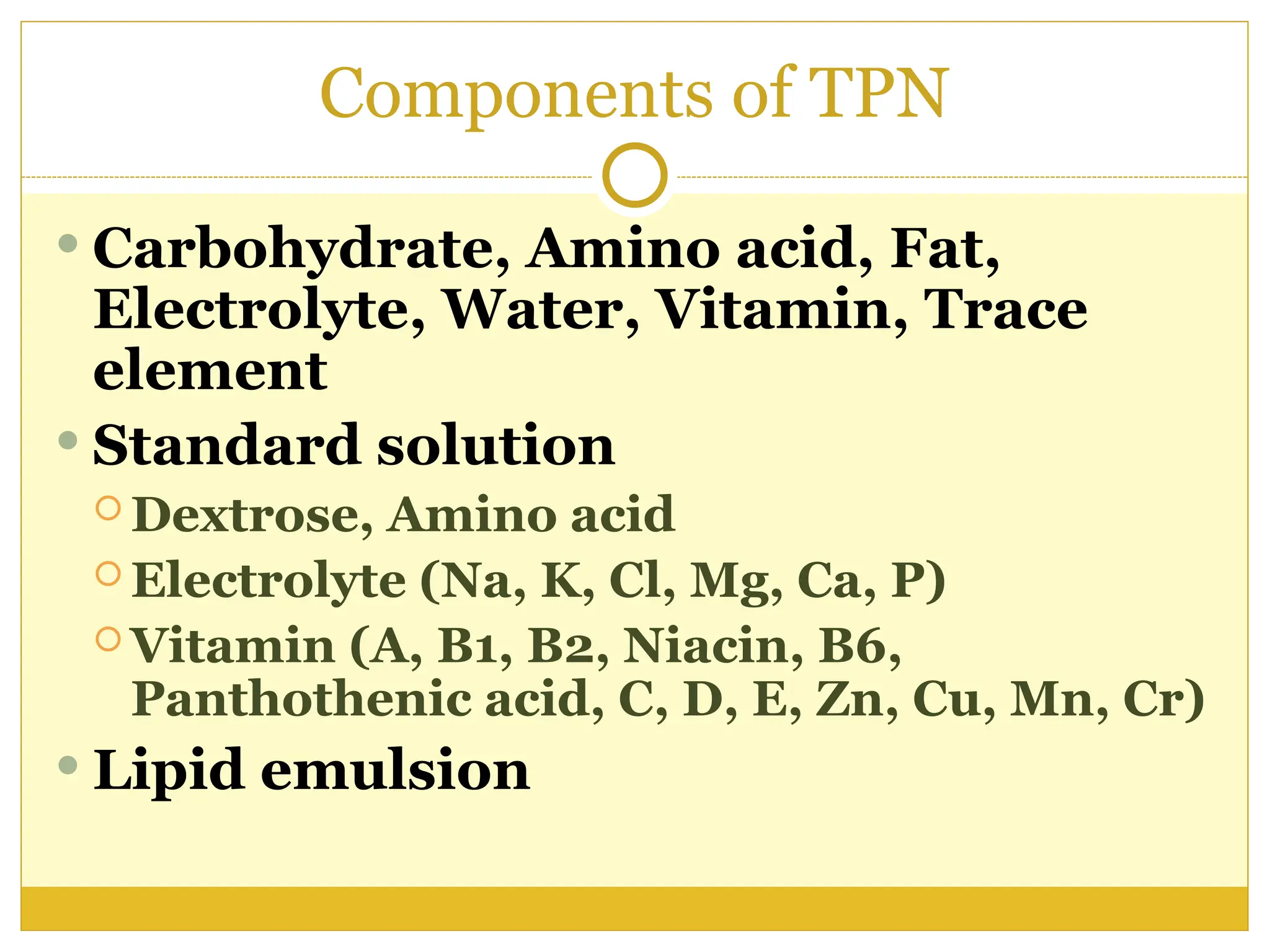
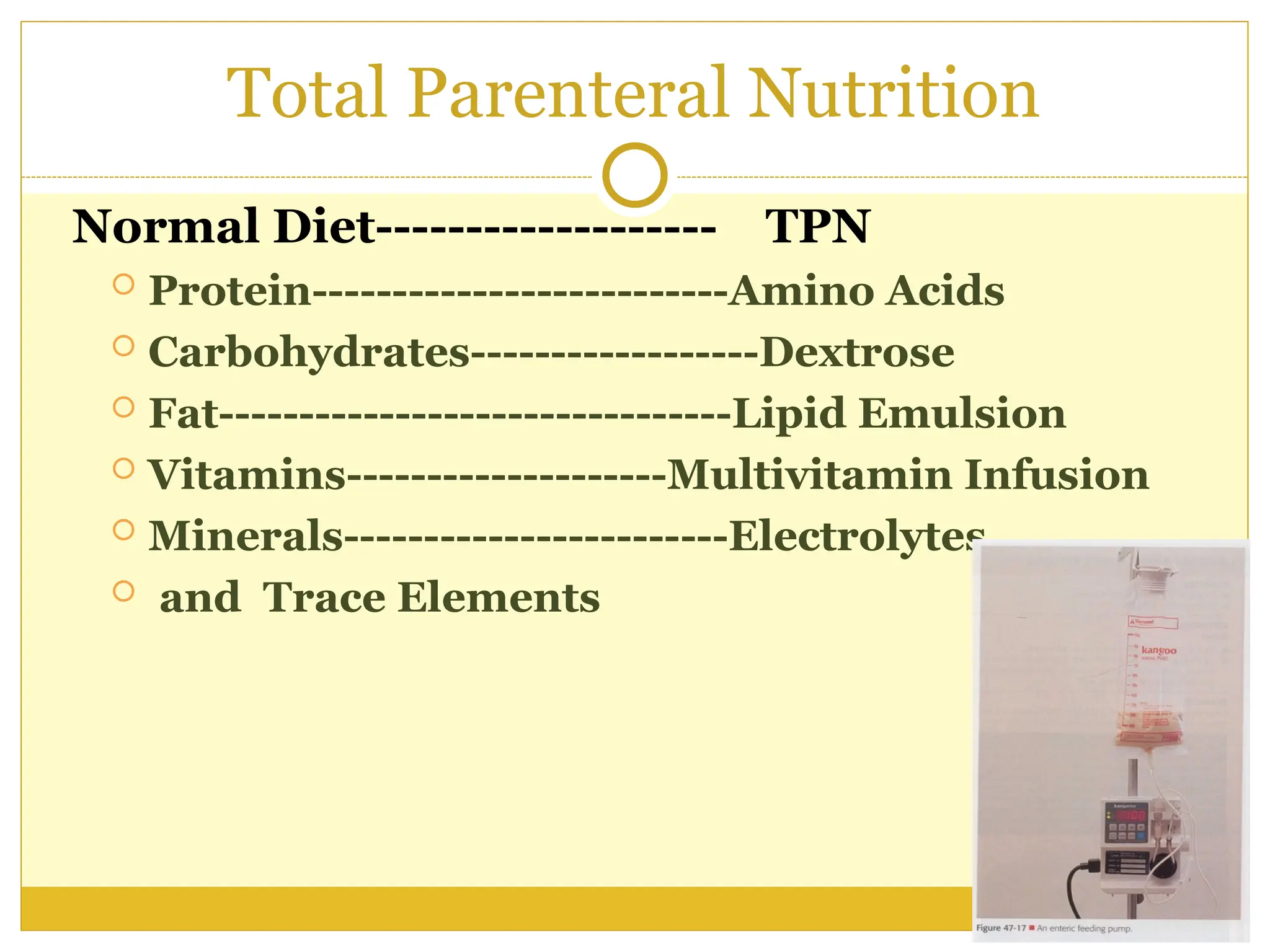
The document outlines the procedures, types, and purposes of nasogastric (NG) tubes, including their insertion, removal, and use for feeding and irrigation. It details the steps for proper placement, confirmation of position, potential complications, and indications for their use in patients unable to eat orally. Additionally, the document covers the protocols for tube feeding, gastrointestinal assessment, and total parenteral nutrition when enteral nutrition is not feasible.